Epilepsy Affects Up To A Third Of People With Autism By Contrast It Affects Only 1 To 2 Percent Of The General Population
Red flags include:
- Disrupted sleep/li>
- Unexplained changes in abilities or emotions
Treatment of epilepsy is crucial to prevent brain damage. If you suspect that you or your child may have epilepsy, seek evaluation from a neurologist. Evaluation typically involves an electroencephalogram to check for seizure-related brain activity.
See these ATN/AIR-P Guidebooks:
Explaining Seizures to Children with Epilepsy and Their Peers
Sometimes it can be difficult for children to understand what is happening when they are having a seizure. In addition, it can be very scary for their peers or friends who witness them. Autism Speaks has put together Visual Stories to explain to children how people with epilepsy are just like everyone else!
Visual Story for Peers of Children with EpilepsyIf a family member suffers from seizures, you may want to consider a medical alert bracelet that can inform first responders of the seizure disorder and any medications that the individual may take. There are a variety of options available on the internet.
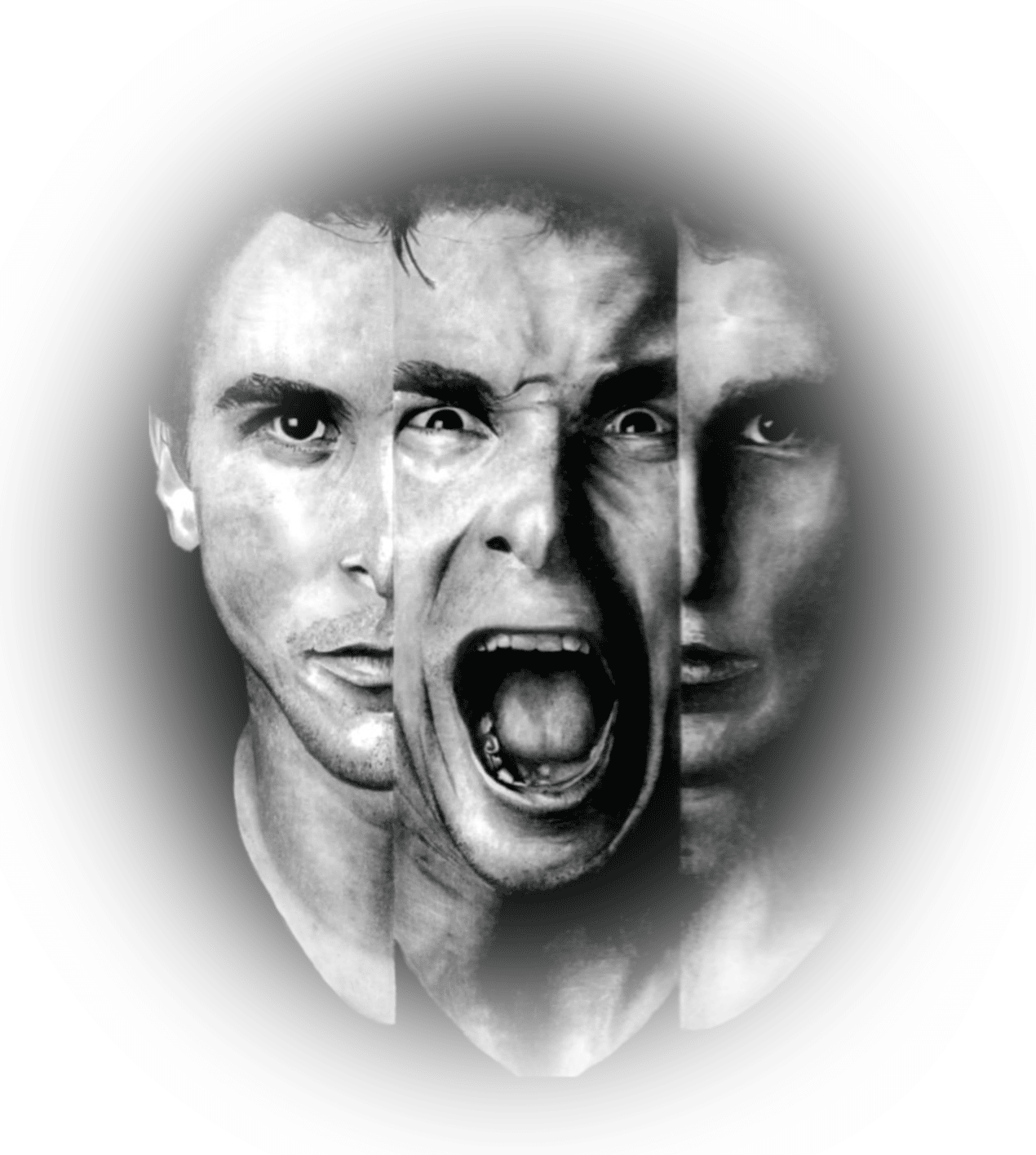
Symptoms Associated With Asd Are Often Misdiagnosed
A study concluded that adult psychiatric service patients with autism are often misdiagnosed. The authors suggest that adult psychiatrists may not be familiar with the diagnosis of ASD. They conclude by saying the high comorbidity rate between schizophrenia and autism may be related to shared neurobiology, but they dont exclude the possibility that arbitrary restrictions imposed by the current diagnostic system also play a part.
Diagnostics have obviously improved in the last decade since this study was published but it does emphasize the importance of diagnostic criteria. If an autistic childs behavior changes suddenly, or if they seem increasingly disconnected from reality, parents should ensure the medical professional they choose to consult with is familiar with both autism and other mental disorders.
While most pediatricians are well versed in areas of mental health, childhood onset schizophrenia in a young patient with autism may require a doctor with diagnostic expertise in developmental disorders and childhood onset schizophrenia.
Could My Autistic Child Be Diagnosed With Schizophrenia Too
For parents dealing with challenging symptoms of autism, research suggesting their child may be at a higher risk of developing schizophrenia could cause unnecessary stress and worry. It is important to note, as mentioned previously, schizophrenia is rarely diagnosed in a child under the age of 12 years.
Even if some of your childs symptoms fit those listed above, your doctor may rule out comorbid schizophrenia or bipolar disorder if the symptoms or behavior is a manifestation of autism. When children go through puberty their behavior changes and challenging autism symptoms may become elevated due to the hormones involved in puberty.
Sensory processing issues found in almost every child with autism may add further difficulty in diagnosing comorbid mental conditions. Sensory impairment sometimes leads to bizarre behavior according to neurotypical standardsthe behavior may seem atypical but the purpose is self-regulation or regulation of the sensory environment.
In addition, repetitive behaviors, a core symptom of children with autism, may be difficult to differentiate from catatonia which is a symptom associated with schizophrenia.
Read Also: Does Caffeine Give You Anxiety
Copy Number Variant And Rare Allele Studies
Autism spectrum disorders such as autism, Asperger’s syndrome and Rett’s syndrome, are developmental psychiatric disorders with high heritability . Over the past few years, genetic studies of ASDs have consistently identified rare and de novo point mutations and large structural variants present in genes encoding interacting synaptic proteins . Such studies have reported co-segregation of putative high-risk alleles with ASDs or performed so-called ‘burden analysis’, in which different alleles of a particular gene are aggregated and the frequency in cases compared with that in controls. Initial studies of ASDs using small samples found rare missense point and structural mutations in the X-linked Neuroligin-3 and Neuroligin-4 genes . Neuroligins are a family of post-synaptic proteins that bind trans-synaptically to a family of pre-synaptic proteins called neurexins. Although these findings were interesting, incomplete penetrance of the mutations and lack of power made the results equivocal. However, missense mutations were subsequently identified in the Neurexin-1 gene at a high frequency in individuals with autism . These suggestive findings have been augmented by the results of recent genomic studies discussed below.
Prodromal Schizophrenia And Autism/ Aspergers Syndrome
Thaker points out that in relation to schizophrenia the negative symptoms, and cognitive, neurophysiological, and functional impairments prece- de psychosis onset by several years. The big issue here is of the difficulty during this period of differentiating Autism/Aspergers Syndrome from these prodromal phenomena of schizophrenia. The old concept of simple schizophrenia of course completely overlaps with Autism/Aspergers Syndrome . The subtype of schizophrenia that is most likely to be confused with Autism/Aspergers Syndrome is the paranoid type.
Carpenter 2009 used the term risk syndrome for psychosis. David 2011 notes a large US cohort with 35% conversion or transition rate within 2. 5 years to full blown psychosis . David 2011 also noted that transition rates decline over time. David 2011 notes the wish to prevent psychosis but that the benefit to harm ratio of a given intervention will be tilted towards harm as false posi- tive rate goes up. There is clearly more research to be done in this area before we can avoid the problems of false positive rates. Autism/Aspergers Syndrome should always be part of the differential diagnosis of Schizophrenia.
Indeed when you look at Eugen Bleulers four key symptoms of schizophrenia all these can occur in Autism/Aspergers Syndrome. Bleuler E. .
Read Also: How To Write About Ptsd
A Model Of Inflammation Leading To Both Shared And Disorder
Under normal conditions, inflammation is controlled by various homeostatic processes that limit or counteract inflammation once it has been induced by an environmental stimulus, e.g. infection . Such control mechanisms ensure that inflammatory processes efficiently remove invading pathogens and contribute to tissue repair and wound healing without placing noninfected, healthy, and unwounded tissue in jeopardy. Dysfunction of such surveillance mechanisms may lead to chronic inflammation, known from numerous pathological conditions such as rheumatoid arthritis, atherosclerosis, obesity, and diabetes .
Figure 1
Can Schizophrenia Be Prevented In Autistic Children
In short, there is no way to prevent schizophrenia.
People with autism do have a greater risk for developing the disorder. There is likely an environmental link for schizophrenia, however. As a result, there are some things that parents can do for autistic children to potentially decrease the odds for the second disorder occurring.
Early intervention for autism is vital to managing the symptoms of the disorder, improving functionality and quality of life, and minimizing the risk of a co-occurring mood or anxiety disorder, such as schizophrenia. Its important to keep stress levels low and emotions regulated.
Early intervention techniques teach children how to cope with stressors and keep themselves calm. This can prevent increased stress from becoming a risk factor for schizophrenia. If a child has undiagnosed autism, their symptoms may worsen, and they may experience added stress from not seeing a reason behind their symptoms.
The best thing to do is to be aware of your childs moods and habits. Alert your childs pediatrician immediately if you notice changes and suspect an issue.
Continue to be an advocate for your child to ensure the right diagnosis is made and treatments are provided. Remember that the earlier you get an accurate diagnosis, the better the long-term prognosis for your child.
Read Also: What Year Was Ptsd Recognized By American Psychiatric Association
Implications For Diagnosis And Treatment/management Strategies
Current classification systems organise ASD and schizophrenia as mutually exclusive diagnoses. Their conceptualisation as neurodevelopmental disorders, in addition to the fact that there are overlaps in symptomatology and cognitive deficits, may prevent clinicians from detecting the potential co-occurrence or continuity of autism and schizophrenia. This means that if an individual develops autism as a young child, they may be less likely to receive a diagnosis of schizophrenia later on, even if psychotic symptoms emerge. Therefore, knowledge about ASD/schizophrenia similarities and distinct characteristics is warranted to inform differential diagnosis and diagnosis of comorbidity. In some patients, it may be more appropriate to take a longitudinal perspective, bearing in mind deviant neurodevelopment with changing predominant clinical features and different intervention needs at different points in life.
Emerging evidence points towards some promising pharmacological interventions that may be useful in treating both ASD and psychotic disorders, since they aim at tackling symptoms such as social and communication impairments or negative symptoms, which are associated with both conditions. They include, among others, oxytocin, cholinesterase inhibitors and glutamatergic drugs, although the evidence base supporting their use in clinical practice is still developing .
Adhd Autism And Schizophrenia Link
A study out of Great Britain has shown that there is a link between, ADHD, autism, and schizophrenia. Scientists have demonstrated that these diseases have a genetic basis, that there are differences in the brain structure which lead to these developmental disorders. The study published in The Lancet and reported in Science Dailyin September, 2010, found that children with ADHD were more likely to have small segments of their DNA duplicated or missing than other children.
These segments are called copy-number variants. Copy-number variants are defined by Wikipedia as are alterations of the DNA of a genome that results in the cell having an abnormal number of copies of one or more sections of the DNA. Apparently, these segments overlap in ADHD, autism, and schizophrenia, which means that ADHD can now be classified as a genetically based disorder like autism and schizophrenia.
Highly sensitive people often have genetically based diseases caused by abnormal fetal development. Studies have shown that there is a direct correlation between the stress experienced by the mother during pregnancy as the creation of an HSP with genetic disorders. Many genetic diseases have existed for a long time in the human race, and as a result, they can be inherited as well.
About Maria Hill
Read Also: What Is The Symbol For Autism
Read Also: Can Energy Drinks Cause Anxiety
Developmental Aspects Continuity And Co
Since the first studies by Rapoport and colleagues, numerous authors have shown that a significant proportion of children and adolescents with psychotic experiences or schizophrenia fulfil criteria for ASD or present with marked developmental abnormalities during childhood . Of note, pre-existing ASD is present in as many as 3050% of patients with childhood-onset schizophrenia and may appear many years before schizophrenia is diagnosed . The same applies to individuals with adult-onset schizophrenia .
Relationship Between Autism And Schizophrenia
The complicated and controversial history linking autism and schizophrenia does little to answer parents concerns about the co-occurrence of these two conditions in their children.
Dr. Eugene Bleuler first used the word autism in the early twentieth century to describe symptoms related to schizophrenia. More specifically, symptoms of withdrawal into an inner worldwhich he had observed in his schizophrenic patients.
This withdrawal, or shutting out of the outside world, is one of the areas where autism and schizophrenia may overlap and cause significant diagnostic difficulty. A childs social withdrawal, accompanied by sensory issues and behavior that may seem like symptoms of psychosis, could leave parents wondering whether the behavior indicates autism or whether childhood onset schizophrenia is a diagnostic possibility.
The two conditions have symptoms and characteristics that may overlap, but there are also many clear differences. While a professional may be able to discern, and diagnose a child according to their symptoms and history, the two conditions are sometimes comorbid and research indicates that those on the autism spectrum may have an elevated risk of developing schizophrenia.
Also Check: What Causes Bipolar Disorder In Men
Is Schizophrenia Part Of The Autism Spectrum
No. Autism isnt part of the schizophrenia spectrum and schizophrenia isnt part of the autism spectrum.
Sometimes autistic people experience symptoms of psychosis if they also live with schizophrenia. Psychosis is not a formal symptom of autism.
Psychosis may be difficult to identify if the autistic person has a limited ability to communicate, though.
In some cases, if a young autistic person experiences psychosis, a clinician may assess for a diagnosis of childhood-onset schizophrenia.
Diagnostic And Behavioral Assessments

ASD Symptoms
ASD symptoms were measured using the ADOS-2 . The ADOS-2 is a gold-standard assessment tool used to assist clinician judgment in making decisions about a possible ASD diagnosis. It is commonly used in ASD research to confirm diagnoses in a standardized manner and to estimate the severity of ASD traits . The ADOS-2 was administered by trained, research-reliable clinicians and consists of semistructured activities and conversations meant to sample a participants real-world social behavior and core autistic characteristics related to language and communication, reciprocal social interaction, imagination and creativity, stereotyped behaviors and restricted interests, and other atypical behaviors. The ADOS-2 algorithm sums across a subset of scored items in order to categorize participants into autism , autism-spectrum , and non-spectrum.
SZ Symptoms
Recommended Reading: Is Level 2 Autism High Functioning
Also Check: Can You Have A Panic Attack While High
Diagnostic Accuracy Of Ados
Sensitivity and Specificity
Table 2 displays the sensitivity, specificity, PPV, and NPV of the ADOS-2, derived by examining the proportions of participants from each subsample whose scores on the ADOS-2 accurately corresponded with the DSM-5 diagnoses determined by all the available information and clinical judgment. The specificity of the ADOS-2 was perfect in TD . Of particular interest for the present study was a high rate of false positives in SZ, yielding a specificity of 56.41%. Seventeen out of 39 participants with a SZ diagnosis met the ADOS-2 criteria for autism or autism-spectrum despite not meeting the DSM-5 criteria for ASD by consensus diagnosis .
Receiver Operating Characteristic Curves
Figure 1 ROC curves predicting DSM-5 diagnostic status based on continuous ADOS-2 algorithm score. ROC curves predicting DSM-5 ASD or SZ diagnostic status based on continuous ADOS-2 negative and positive symptoms. ROC curves predicting DSM-5 ASD or SZ diagnostic status based on continuous PANSS Negative and Positive symptoms. ASD, Autism Spectrum Disorder SZ, Schizophrenia TD, Typical Development.
Schizophrenia And Autism: Separate Entities Or Pieces Of The Same Puzzle
Schizophrenia and autism seem to overlap at multiple levels. Therefore, it is not surprising that autism was initially believed to be an early manifestation of schizophrenia, and as such it was often referred to as childhood psychosis or schizophrenic syndrome of childhood . In 1971, ASD was finally separated conceptually from schizophrenia based on a delineation of symptomatic differences , family histories, and differential treatment responses in individuals with suspected adult schizophrenia versus infantile autism .
At the behavioral level, deficits in social interaction and cognition, disruption of emotional processing and sensorimotor gating, and impairments in executive functions are psychopathological features commonly observed in both disorders . Moreover, at least a subset of individuals with autism frequently experience psychotic phases involving auditory and visual hallucinations, similarly to acutely ill patients with schizophrenia . Based on this, it has been suggested that individuals with autism are at increased risk of developing psychosis and that the presence of neurodevelopmental deficits typically associated with autism may represent an alternative entry-point into a common final pathway of psychosis .
Read Also: What Do We Know About The Inheritance Of Ptsd
The History Of The Connection Between Autism & Schizophrenia
The link between schizophrenia and autism goes back many years. Historically, autism was considered a feature or symptom of schizophrenia. It was not until 1943 that it was even considered to possibly be its own disorder.
The negative symptoms of schizophrenia, such as flat affect, social withdrawal and detachment, communication difficulties, little interest in other people and preference instead for objects, and rigid and repetitive behaviors were actually autistic traits.
Research in the 1970s showed that hallucinations, which are a common psychotic symptom of schizophrenia, were not common in children with autistic traits that manifested prior to age 3. Instead, these children often turned out to have difficulties with social relationships and language delays.
Finally, in 1980, autism and schizophrenia were recognized as two separate diagnoses with a big distinction age of onset. Children presenting with symptoms around age 4 or earlier were considered to have autism, while those with symptoms that began between the ages of 16 and 30 had schizophrenia.
In the 1990s, research began to shift the landscape again, indicating a potentially greater connection between the two disorders. It is now recognized that it is possible to have both schizophrenia and autism at the same time. This situation is called comorbid disorders.
Regarding Correlation Of Illness Duration Of Schizophrenic Parents And Autism Quotient Scores Of Their Offspring
In this study, there is a weak positive correlation between duration of illness of schizophrenic parents and AQ meaning AQ scores will increase when the duration of schizophrenia illness increase but this correlation is with no statistical significance . This non-significance may be due to the small sample size of our study this point can be overcome in the future research. Unfortunately, we did not find any study that approached this point of correlation.
You May Like: How To Get Rid Of Ptsd Anxiety
Autism Schizophrenia Linked To Environmental Pollution According To New Study
A new study reveals that exposure to environmental pollution may cause autism or schizophrenia.
While the link pollution and autism has previously been investigated, researchers from the University of Rochester have uncovered the biological mechanism that may explain how pollution can put people at a higher risk for both autism and schizophrenia.
From a toxicological point of view, most of the focus of air pollution research has been on the cardiopulmonary system the heart and lungs, study author Deborah Cory-Slechta, professor of environmental medicine at the University of Rochester, told FoxNews.com. But I think its becoming increasingly clear that the adverse things happening there are also happening in the brain, and this may be adding to risks for neurodevelopmental disorders like autism that we hadnt thought about before.
To conduct the experiment, Cory-Schleta and her colleagues exposed a group of baby mice to levels of air pollution equivalent to those seen in rush hour traffic.
After four hours of pollution exposure during two four-day periods, the group of mice exposed to pollution exhibited significant changes in behavior compared to mice living in an environment with clean hair.
That kind of air pollution produces inflammation, it is going to produce inflammation peripherally and in the brain as well. And when you produce inflammation in the brain, you can kill cells there, Cory-Slechta said.