What Are Brain Scans
A brain scan is a general term that covers a diverse group of methods for imaging the brain. In psychiatric clinical practice, brain scans are mostly used to rule out visible brain lesions that may be causing psychiatric symptoms.
However, in research we use them to learn about the pathologies of the brain in mental illness. A common method is magnetic resonance imaging that allows us to look at the changes in the volume and structure of different areas of the brain, and integrity of the pathways connecting them.
Then there is functional MRI . This method examines blood flow in different areas of the brain as a measure of their dynamic function, mostly in response to a task or event, such as thinking about trauma or viewing of a trauma-related image. I use fMRI in my research to look at the brain circuitry involved in how people can be instructed to learn fear and safety. Positron emission tomography, or PET, and single photon emission CT, or SPECT, are also used in looking at brain function.
At the current stage of the technology and research, psychiatrists, psychologists and neuroscientists only use these methods for researching the brain changes in mental illness, and not for making diagnoses. In other words, we have to combine data from tens of people with a mental illness to determine how, on average, different areas of their brain may differ in volume or function from others.
Neural Circuits In Women With Abuse And Ptsd
PTSD subjects had increased symptoms of anxiety, fear, dissociation, distress, substance use disorders , and PTSD at all time points during both study days relative to non-PTSD. Acquisition of fear was associated with increased skin conductance responses to CS exposure during the active versus the control conditions in all subjects. There was increased SC for PTSD during the first CS-UCS presentation. Extinction of fear was associated with increased skin conductance responses to CS exposure during the active versus the control conditions in all subjects. When PTSD and non-PTSD subjects were examined separately, SC levels were significantly elevated in non-PTSD subjects undergoing extinction following the active compared with the control condition during session one.
Control Of Magnetic Power
An MRI machine is used to create a three-dimensional image of a corporal component with electric currents and radio waves of a mental illness disease. Its technology is complex and tough to understand. Nevertheless, a man who passes an MRI machine is fired with a series of radio waves, which affects the bodys tissues. These radio waves produce a picture, which perhaps contains information about how much energy every tissue produces in the body.
The arteries and veins can be seen with an MRI machine. There is the fact that standard MRI cannot see flowing fluid, like blood running in an artery. The machine can see the arteries and veins due to a contrast dye injected into the bloodstream. Tumors and arteriovenous malformations are treated with comparison as well. It is relatively easy to obtain such details because an MRI machine is ordinarily complete in about an hour or two. Its not enjoyable for the person on this MRI machine because the magnets appear noisy. They toggle on and off and appear to be just a few centimeters away from a persons nose. In the meantime, most MRI machines need people to sit in small tubes and keep themselves silent. Sometimes mental illness patients find it challenging to endure the entire experience.
Often people go to an MRI because they have unexplained behaviour changes due to mental illness, and they dont know why these changes occur.
Yet it may be worth spending an hour in an MRI machine because the patient wants information about:
You May Like: How Do You Know If You Have Postpartum Depression
Why Choose Amen Clinics For Treating Ptsd
Most psychiatrists never look at the brain and make their diagnostic assessment based only on a patients reported symptoms, which is why many people are misdiagnosed or prescribed the wrong treatment. SPECT scans are very helpful in determining whether a patient has PTSD or another disorder. A research study conducted at Amen Clinics evaluated the brain blood flow patterns in TBI and PTSDtwo conditions that have many overlapping symptoms. The study found that brain SPECT imaging was able to differentiate the two conditions with 89% accuracy. This research was recognized by Discover Magazine as #19 of the top 100 science stories of 2015. At Amen Clinics, a comprehensive evaluation that includes brain SPECT imaging paves the way for people with PTSD to get an accurate diagnosis and more effective treatment that leads to faster healing.
How Do We Diagnose Ptsd
Like most other psychiatric conditions, PTSD is a clinical diagnosis. That means psychiatrists diagnose PTSD by the symptoms presented by the patient. Clinicians look for a constellation of symptoms for a diagnosis:
- history of exposure to trauma
- intrusive symptoms such as frequent flashbacks, nightmares, intrusive memories
- avoiding any reminder of trauma and its memories
- hyperarousal, or being overly vigilant, having sleep disturbances, being easily startled
- negative thoughts or feelings
- significant distress or dysfunction.
When enough number of the above criteria is met, a clinician makes a diagnosis of PTSD.
We clinicians and researchers use the above criteria for consistency in research. We want to be sure that what we call PTSD across different studies passes the threshold of a certain severity and diversity of symptoms.
However, effects of trauma may not reach the diagnostic threshold for PTSD, but can still be very stressing. A traumatized person who has frequent nightmares and flashbacks and avoids leaving their house out of fear, is seriously stressed even though they may not meet the required number of negative symptoms per the diagnostic manual. From a clinical perspective, we still address their symptoms and treat them. In other words, what matters in clinical practice is helping with the symptoms that are distressing and cause dysfunction.
Don’t Miss: What Are The Possible Causes Of Eating Disorders
What Are The Limitations Of Mri Of The Head
High-quality images depend on your ability to remain perfectly still and follow breath-holding instructions while the images are being recorded. If you are anxious, confused or in severe pain, you may find it difficult to lie still during imaging.
A person who is very large may not fit into certain types of MRI machines. There are weight limits on the scanners.
Implants and other metallic objects can make it difficult to obtain clear images. Patient movement can have the same effect.
A very irregular heartbeat may affect the quality of images. This is because some techniques time the imaging based on the electrical activity of the heart.
MRI is generally not recommended for seriously injured patients. However, this decision is based on clinical judgment. This is because traction devices and life support equipment may distort the MR images. As a result, they must be kept away from the area to be imaged. Some trauma patients, however, may need MRI.
Although there is no reason to believe that MRI harms the fetus, pregnant women should not have an MRI exam during their first trimester unless medically necessary.
MRI may not always distinguish between cancer tissue and fluid, known as edema.
MRI typically costs more and may take more time to perform than other imaging methods. Talk to your insurance provider if you have concerns about the cost of MRI.
Dont Miss: How To Handle Eating Disorders
How Is Ptsd Diagnosed
Doctors may look for a combination of factors when diagnosing PTSD, including the patients history, symptoms, and behaviors. Beyond assessing these factors, however, its possible an MRI could be used to help confirm or predict PTSD. For example, scientists have identified alterations in brain areas such as the hippocampus, prefrontal cortex, and amygdala in people with PTSD and other psychiatric disorders. Those who have experienced traumatic brain injury may also be particularly good candidates for having an MRI for PTSD.
The symptoms and cognitive changes that arise from PTSD are not fully understood. With the ability to better examine and even predict the effects of PTSD through MRIs, doctors may be able to improve patient outcomes.
Read Also: How To Deal With Ptsd Triggers
The Most Discriminative Regions
Brain regions with the most discriminative power between groups were identified in both brain hemisphere and all the four lobes , which mean there were widespread regional alterations across the whole brain in PTSD patients as well as TEC subjects.
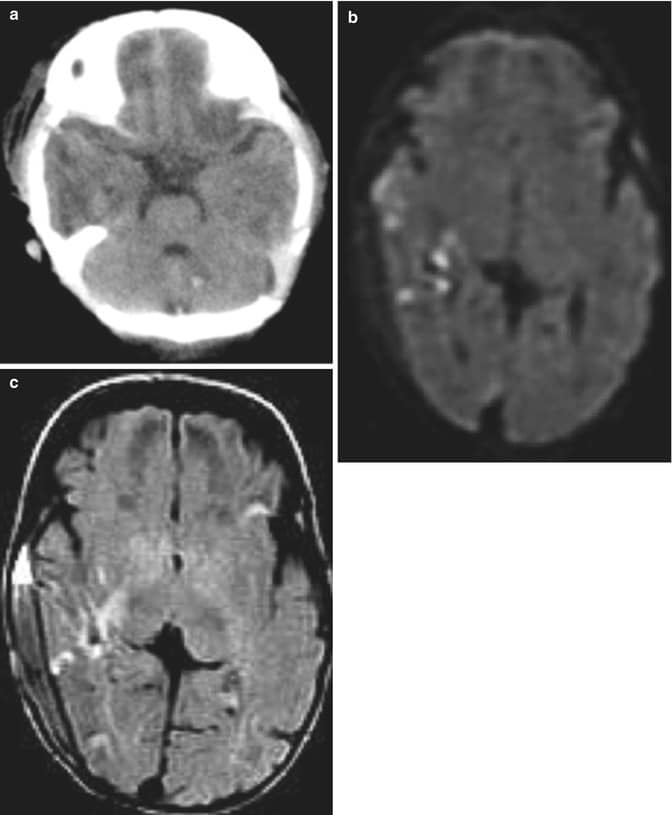
Figure 3. Brain regions that showed the highest discriminative value for the classification in PTSD and HC, TEC and HC, and PTSD and TEC. Regions were identified by setting the threshold to 30% of the maximum weight value. Red, blue, and green colors indicate the most discriminative regions of GMV, ALFF, and ReHo features, respectively.
In comparison of PTSD and HC, regions displaying most difference in GMV appeared in the bilateral middle occipital gyrus, right inferior parietal lobule, left superior frontal gyrus, right cerebellum, and the bilateral middle frontal gyrus ALFF difference mainly exhibited in the right precuneus, left temporal pole , left calcarine fissure, right caudate nucleus, and the left superior frontal gyrus ReHo difference appeared in the right temporal pole .
In the comparison of PTSD and TEC, GMV difference mainly included the bilateral middle temporal gyrus, right rolandic operculum, right superior frontal gyrus, and the left postcentral gyrus ALFF difference were shown in the left lingual gyrus and left precuneus gyrus ReHo difference mainly exhibited in the right precuneus gyrus .
Normal Development Of The Brain Across The Lifespan
To understand how traumatic stress occurring at different stages of the life cycle interacts with the developing brain, it is useful to review normal brain development. The normal human brain undergoes changes in structure and function across the lifespan from early childhood to late life. Understanding these normal developmental changes is critical for determining the difference between normal development and pathology, and how normal development and pathology interact.
Although the bulk of brain development occurs in utero, the brain continues to develop after birth. In the first 5 years of life there is an overall expansion of brain volume related to development of both gray matter and white matter structures however, from 7 to 17 years of age there is a progressive increase in white matter and decrease in gray matter while overall brain size stays the same.13–16 Gray matter areas that undergo the greatest increases throughout this latter developmental epoch include frontal cortex and parietal cortex.17,18 Basal ganglia decrease in size, while corpus callosum,19,20 hippocampus, and amygdala21–23 appear to increase in size during childhood, although there may be developmental sex-laterality effects for some of these structures.24 Overall brain size is 10% larger in boys than girls during childhood.24
Read Also: Did Marilyn Monroe Have Schizophrenia
Intracranial And Brain Volume
Intracranial volume was reduced in PTSD patients in the main region-of-interest analysis as well as in PTSD patients compared with traumatized control subjects. Total intracranial volume stabilizes in early adolescence and provides an estimate of premorbid brain volume . Thus, smaller intracranial volume in PTSD may indicate abnormal brain development before or during early adolescence. Consequently, reduced intracranial volume may be a risk factor for PTSD and may be associated with trauma susceptibility. Total brain volume was also significantly smaller in PTSD patients compared with all control subjects, nontraumatized control subjects, and traumatized control subjects but not in the comparison between traumatized and nontraumatized control subjects. These results suggest that brain volume reductions in PTSD patients are related to the disorder itself rather than the exposure to trauma. In addition, our comparison with depression suggests that total brain volume reduction is a more specific marker for PTSD than is hippocampal volume.
Database Of Imaging Studies In Ptsd
Published studies that measured brain structure using MRI in patients with PTSD and a control group were included in the database. A MEDLINE search of studies published from 1992 through June 2016 was performed, combining Medical Subject Heading terms and free text searches. A total of 800 publications were identified, of which 113 met inclusion criteria and were included in the database. Further details, including search terms and a study inclusion flow chart , are provided in the online supplement.
Recommended Reading: Are You Happy Lyrics Bipolar Sunshine
The Association Between Dementia And Ptsd
One study shows that veterans with PTSD were at much higher risk of developing dementia than were veterans without the disorder. The study also shows that the risk varies according to the medications the study participants were taking. Those taking psychotropic medications, such as antidepressants, anti-anxiety drugs and mood stabilizers, were at higher risk for developing dementia than were those who did not take these medications.
Older adults and veterans with dementia may exhibit more symptoms of PTSD according to the Veterans Administration .
Conversely, PTSD may be a risk factor for dementia. In fact, results from a large VA cohort study show that people diagnosed with PTSD were nearly twice as likely to develop dementia that were those not diagnosed with the disorder.
Gary Martin Hays & Associates: Helping Brain Injury Victims
Normal MRIs and CT scans can fail to find evidence of a large majority of brain damage. While you may feel confused or helpless at first, the important thing is to not give up. It’s vital you receive a correct brain injury diagnosis so that you can receive all the medical treatment, rehabilitation, and compensation you need to recover.
Whether your injury happened at work, because of an assault, or during a car or motorcycle accident, our attorneys and case managers can help you find the right doctors to help treat your brain injury.
If you have questions about traumatic brain injuries and your legal rights after a wreck or work injury, contact us online or at 934-8000 for a free evaluation of your case.
FURTHER READING:
Don’t Miss: How To Treat Depression And Anxiety
Current And Future Functional Imaging Techniques For Post
Alisha Prasada, Ardalan Chaichia, D. Parker Kelleyb, Joseph Francis*b and Manas Ranjan Gartia*aaDepartment of Mechanical and Industrial Engineering, Louisiana State University, Baton Rouge, LA 70803, USA. E-mail: bComparative Biomedical Sciences, School of Veterinary Medicine, Louisiana State University, Baton Rouge, LA 70803, USA. E-mail:
First published on 8th August 2019
Cognitive Function And Brain Structure In Ptsd
Studies in PTSD are consistent with changes in cognition and brain structure. Multiple studies have demonstrated verbal declarative memory deficits in PTSD.53,106–108
The meaning of findings related to deficits in memory and the hippocampus in PTSD, and questions related to the relative contribution of genetic and environmental factors, has become an important topic in the field of PTSD and stress research. There are three possible models, taking into account genetic or environmental factors, which have been proposed to explain smaller hippocampal volume in PTSD: Model A , Model B , and Model C .166–169 In Model C , smaller hippocampal volume represents a premorbid risk factor for PTSD. In support of this model Pitman and colleagues170 have demonstrated that lower premilitary IQ is associated with combat-related PTSD, as well as finding a correlation between PTSD symptoms and hippocampal volume in twin brothers.151 Model A states that stress leads to damage or inhibition of neurogenesis via hypercortisolemia, decreased BDNF, or increased glutamate. Model B states that a combination of environmental and genetic factors leads to deficits in hippocampal function and structure. Showing that an intervention like medication changes hippocampal volume and cognition would provide support for at least a partial contribution of the environment to the outcomes of interest.
You May Like: How Does Cbd Help Ptsd
Brain Imaging Predicts Ptsd After Brain Injury
Post-traumatic stress disorder is a complex psychiatric disorder brought on by physical and/or psychological trauma. How its symptoms, including anxiety, depression and cognitive disturbances arise remains incompletely understood and unpredictable. Treatments and outcomes could potentially be improved if doctors could better predict who would develop PTSD. Now, researchers using magnetic resonance imaging have found potential brain biomarkers of PTSD in people with traumatic brain injury .
The paper, Smaller Regional Brain Volumes Predict Post-Traumatic Stress Disorder at 3 Months after Mild Traumatic Brain Injury, was recently published in Biological Psychiatry: Cognitive Neuroscience and Neuroimaging. McGowan Institute for Regenerative Medicine affiliated faculty member David Okonkwo, MD, PhD, Professor of Neurological Surgery and Director of the Neurotrauma Clinical Trials Center, Director of Neurotrauma and of the Scoliosis and Spinal Deformity Program at UPMC, and the Clinical Director of the Brain Trauma Research Center, is a co-author of this work.
The researchers followed over 400 such TBI patients, assessing them for PTSD at 3 and 6 months after their brain injury. At 3 months, 77 participants, or 18 percent, had likely PTSD at 6 months, 70 participants or 16 percent did. All subjects underwent brain imaging after injury.
Read more
Molecular Cellular And Behavioral Indicators In Ptsd
| Fig. 2 Different biomarkers of PTSD. HPA: hypothalamic pituitary adrenal SAM: Synergistic Activation Mediator ACTH: adrenocorticotropic hormone CRF: corticotropin hormone releasing factor GCR/GR: glucocorticoid receptor BDNF: brain-derived neurotrophic factor GABA: Gamma-Aminobutyric Acid FKBP5 SERT: serotonin transporter or 5-HTT DAT: dopamine transporter gene rRNA: ribosomal ribonucleic acid ApoE4: apolipoprotein E H3K27: trimethylated histone H3 lysine 4 amino acid GFAP: glial fibrillary acidic protein IL: interleukin TNF: tumor necrosis factor I NK: Natural Killer cells Th: T-helper cells. |
Also Check: Does Bipolar Get Worse With Stress
Neuroscientists Say Brain Scans Can Spot Ptsd
To revist this article, visit My Profile, then View saved stories.
Post-traumatic stress is estimated to afflict more than 300,000 veterans of Iraq and Afghanistan, but until now, it’s been labeled a “soft disorder” — one without an objective biological path to diagnosis. That may have changed this week, after researchers at the University of Minnesota and the Minneapolis VA Medical Center announced they’d found a distinct pattern of brain activity among PTSD sufferers.
The team used a brain imaging method called magnetoencephalography , which measures how the brain processes information. They scanned the brains of 74 U.S. veterans with PTSD, and 250 civilians without the disorder. By spotting specific brain biomarkers, they said they0 managed to accurately diagnose PTSD sufferers with 90 percent accuracy.
MEG machines are a fast, sensitive and accurate way to measure electric activity in the brain. Whereas CT scans and MRIs record brain signals every few seconds, MEGs can do it by the millisecond, catching biomarkers and brain activity that the other tests inevitably miss.