Statistics On The Growing Nursing Shortage In The Us
A review of studies on appropriate nurse staffing conducted by the Patient Safety Network established a direct connection between adequate nurse staffing levels and patient safety. The less time nurses can spend at a patients bedside, the higher the risk to the patient. In addition to nursing shortages, a surge in COVID patients would increase work load for staff and decrease time spent with patients.
- The Associated Press reported that staffing at the emergency room of a hospital in Michigan was hampered by recent nurse departures, requiring that each of the five nurses on duty care for four patients at one time.
- A survey conducted by McKinsey found that 22% of nurses were thinking of leaving their current position. Of the nurses considering a job change, 60% said they were more likely to quit due to the COVID pandemic.
- The primary reason nurses gave for wanting to leave was inadequate staffing , followed by the intensity of the workload and other demands and the emotional toll of the work .
- The U.S. Bureau of Labor Statistics estimates that there will be 194,500 openings for registered nurses each year on average over the next decade.
- ANA reports that about 500,000 experienced RNs will retire in 2022, requiring about 1.1 million new RNs to replace those retiring as well as to fill new RN positions.
Why Are Nurses Experiencing Ptsd
According to the National Center for Biotechnology Information , posttraumatic stress disorder is the fourth most common psychiatric disorder in the United States.2 However, the nursing workforce is increasingly susceptible.
An article in the New York Times reported that as many as 28% of military and civilian nurses experience PTSD at some point in their careers when:3
- Caring for severe wounds on a regular basis
- Witnessing death and having end-of-life conversations
- Offering continual support to individuals and their families
- Experiencing verbal or physical abuse from distraught or unstable patients
- Being constantly exposed to germs and contagious illnesses
Additionally, while anyone can get PTSD, women are twice as likely as men to develop the disorder. A 2019 American Community Survey estimated that while there are roughly 300,000 male registered general nurses, female general nurses far surpass that number at just over 2 million, which may point to the prevalence of PTSD within the nursing profession.4
However, there are many other factors that play a role in the development and diagnosis of PTSD, including:
- Biological traits such as genetics
- Past experiences such as childhood trauma
- Pre-existing conditions such as depression, anxiety, or substance abuse
Suicide Rates Have Risen Amongst Nurses
Prior to the pandemic, nurse suicide rates were at an all-time high. Researchers found higher rates of suicide among both women and men working in nursing when compared with non-nurses.
- Suicide incidence was 11.97 per 100,000 people among female nurses and 39.8 per 100,000 among male nurses.
The World Health Organization reports that one person dies every 40 seconds by suicide and it is the 10th leading cause of death in the United States. Its a silent epidemic that until recently was rarely talked about.
In the aforementioned study, nurses were more likely to have,
- Reported mental health problems,
- History of treatment for mental illness,
- History of previous suicide attempt,
- Leaving a suicide note, and physical health problems than the general population,
- Men were more likely to successfully carry out the attempts.
And this was before nurses were working 60+ hours a week, holding the hands of patients dying without their loved ones, communicating via iPad with families, and being separated from their spouses, children, and family for weeks on end.
If youre having thoughts of suicide the National Suicide Prevention& Crisis Hotline can help, .
Since COVID-19, there has been an increased spotlight on nurses mental health. The psychological scars of the stress, death, lack of PPE, and isolation will impact the nursing profession long beyond the physical effects.
You May Like: Which Organization Sets The Standards For Diagnosing Eating Disorders
The Development Of Ptsd And Ptsd In Nurses Today
As the label has evolved, the diagnosis of PTSD now includes the aftereffects of trauma associated with domestic abuse, war-zone reporting, and vicarious trauma. Loss of sleep, nightmares of the event, irritability, and frequent startling to minor noises are all well-publicized symptoms, which, if lasting more than six months, are considered diagnosable as PTSD. â
Other lesser-known and easily missed symptoms of nurses with PTSD can include a form of hyper-vigilance where the nurse is hyper-focused on stable patients, being irritable or frequently angry, and feeling detached from friends and family. â
Another subtle symptom is the nurse with an exaggerated negative belief: “If I were a better nurse, then I would have caught that patient’s decline.” Difficulty concentrating, avoiding certain rooms where they experienced trauma, and non-specific somatic complaints such as body aches, headaches, and lack of overall energy. Nurses with PTSD may be calling out sick more often as a protective mechanism.
And with increasing reports of a nursing shortage in the US, American nurses are only going to have more pressure put on them.
Not all people who experience the same trauma event end up with symptoms of PTSD.â
Causes And Risk Factors Of Post

Stressful events in the patients life, including the degree of trauma theyve experienced, are grounds for PTSD development. Other causes include:
- Being predisposed to a risk factor including having a family history of mental illness
- Individuals with temperamental traits
- Brain activity and response to a traumatic event
These factors will likely determine the risk of developing PTSD after a traumatic event, and these include:
- Suffering from severe or long-term trauma
- Impacted mental health or having conditions such as anxiety or depression
- Working in a career that exposes one to stressful occurrences
- A lack of a strong family and social support system
Recommended Reading: Prodromal Symptoms Of Schizophrenia Are Evident:
Nurses Supporting Nurses Through The Professions Ptsd Crisis
Nurses are on the front line in the battle against COVID-19. In addition, they play many other important roles in helping communities, families, and individuals protect themselves and return to wellness. To meet the expectations others set for them and they set for themselves, nurses must perform at their peak. Doing so requires recognizing when stress and trauma are causing them to feel symptoms associated with PTSD.
Nurses and other health care professionals are responding to the epidemic of PTSD in the profession via education, treatment, and other support services. Nurses health is the key to improving patient outcomes, supporting the profession, and promoting the health of individuals and communities.
Risk Management Of Ptss
A body of evidence has shown that training should also be targeted at improving a supportive work environment. Therefore, according to existing literature, hospital management and supervisors need to anticipate the effects of traumatic exposure by training HCWs in evidence-based anticipatory methods of coping with stressful events, in reducing the development of post-traumatic stress reactions and general distress, and in educating HCWs to support their colleagues after adverse events . A study by Zhang et al. showed that simple standardized questionnaires can be used, which should be supplemented with a brief questionnaire assessing work conditions . A description of a protective program has been published by Cao et al. based upon hands-on recent experience in China. An important part of that program was the repeated use of a short questionnaire supplemented with personal interviews with a representative group of employees.
Recommended Reading: Side Effects To Pristiq
Demands For Resources Largely Ignored For Decades
A particularly big part of insufficient resource trauma comes from inadequate nurse staffing levels, which may lead to bad outcomes for both nurses and patients. The evidence for these outcomes, both compelling and consistent worldwide, is based on more than two decades of research. Having to forego what you know is right when theres just not enough staffing in a high-stakes environment feels like a betrayal of ones spirit. A nurses sense of morality, of what is right and wrong, is endangered.
More recently, there has been a shortage of PPE throughout US hospitals. But I know nurses who were told by employers to take care of Covid-19 patients regardless of whether or not adequate PPE was available. Clearly this was a danger to both nurses and patients surely this qualifies as a traumatizing experience.
Other nurses some new, some working previously in non-acute care have been deployed to critical care units. Understanding the technology of these complex environments requires a steep learning curve. The knowledge, then, to competently care for these patients may be considered an insufficient resource.
The Effect Of A High Hospital Covid Death Toll On Nurses
We all fear the day when one of our patients suffer a cardiac or pulmonary arrest under our care. Shares Tina, a newer nurse who is just two years into her nursing career. We know sooner or later in our career we will all have to call a code blue to one of our patients rooms. Watching them die unexpectedly is really a hard thing to do. Its one thing when your patient is on palliative care or is a DNR and you know that death is coming. In that circumstance our job is to keep them comfortable and help their family get closure. We have a role during their death, so we feel we provide effective care even if that means we are only making them comfortable. When a patient who is doing well unexpectedly dies that is a whole different story because that is not supposed to happen. That is really hard on us. Luckily, on the regular nurses floors that does not happen often. Covid changed all of that for us. We are left spinning as otherwise healthy patients are dying daily with most days we have multiple deaths in our unit. We dont have time to process a death because if we arent on top of our other patients, they may very well follow suite. concluded Tina as she paused to catch herself from crying.
Recommended Reading: Feritriphobia
Why Is Mental Health Important For Healthcare Workers
Many things can go hand-in-hand with poor mental health, such as poor quality sleep, a lack of engagement, reduced concentration and focus, and our ability to handle stressful situations. Whether it is long-term stress , anxiety, depression, vicarious trauma, or PTSD, the impact that mental health has on our physical and emotional functions can be far reaching. Poor mental health can affect all areas of our lives, not just our working abilities it impacts how we act, think and feel.
When we consider the working life of a healthcare worker, they likely work stretches of long days or nights, have many patients to care for, are under-resourced, and are often faced with unexpected events. To provide high-quality, safe care during such circumstances requires a good level of focus, quick responses, critical thinking and countless empathy, all of which are hard to achieve when experiencing poor mental health.
Taking care of workers mental health is vital, to not only limit absenteeism, but to also ensure the staff present are able to work to the best of their ability. Ensuring their actions are safe, that the care they provide is of a high standard, and that the patients and their families benefit from an efficient and engaged workforce is key.
Features Of The Questionnaire
The questionnaires consisted of items regarding demographic variables and information about the work environment. The following four validated surveys were also included in the survey:
The Hospital Anxiety and Depression Scale is a 14-item self-report screening scale originally developed to indicate the possible presence of anxiety and depression states in the setting of a medical, nonpsychiatric outpatient clinic. HADS consists of a 7-item anxiety subscale and a 7-item depression subscale. A score of > 8 identifies those with a positive history for anxiety and/or depression . The validity of the HADS has been extensively studied for identifying anxiety and depression disorders in a variety of populations including the general population, general practice and psychiatric patients .
We included a variety of questions asking the nurses how the felt about their work environment. The responses of the nurses to these questions were scored used a 5 point Likert scale from never to very likely. We asked the nurses if they had nightmares or anxiety related to their job description or environment. If nurses reported symptoms of nightmares or anxiety, they were asked to identify the primary work related trigger associated with each symptom.
You May Like: Anxiety And Burning Sensation
Why Nurses Experience Ptsd
The environment in which nurses work puts them at risk for “triggers and traumas of PTSD,” according to Mealer. “Nurses see people die. They work on resuscitating patients. They try to control bleeding. They have end-of-life discussions,” Mealer said. She added, “And sometimes they are verbally or physically abused by patients or visiting family members.”
Nurses across many care settings are vulnerable to PTSD, Mealer said. In some settings, the risk may be higher than in others. For instance, a study in the Journal of Heart and Lung Transplantation recently found that up to 48% of nurses in a critical care unit meet the criteria for PTSD.
Lucchesi reports that burnout for some specialties may be higher, too.
How Ptsd Is Hurting Nursing
Every time I hear that there is a nursing shortage in America, I feel myself cringe. There is not a shortage of nurses in America. There is a shortage of nurses who choose to work at the bedside. There is a reason, and it is called post-traumatic stress disorder.
Medically, we have learned that PTSD can occur after a single event or as a result of chronic stressors for a period of time. As a living organism, we know that the body can only sustain so much stress before it starts to break down. These ailments can be physical and/or mental. Sometimes they happen over a period of time, however often times we do not even realize the symptoms until they have forced us to take notice. As a nurse, I know when our bodies have had enough, and they need to rest, they will make us rest.
Bedside nursing is hard and very stressful. The bedside nurse is responsible for caring for multiple people every minute of every shift. That is, multiple sick and potentially dying people. The nurse is responsible for monitoring the patients response to treatment, the patients condition, the patients mental health, the doctors orders, assisting the patient with activities of daily living, and being there for the family.
Bedside nurses are the coordinators of care. We are the ones who make sure that all parts of the care plan are being carried out and that the system is working the best it can. We are the ones who comfort the patients when they need us the most.
We get scared.
Don’t Miss: Gossip Girl Blair Bulimia
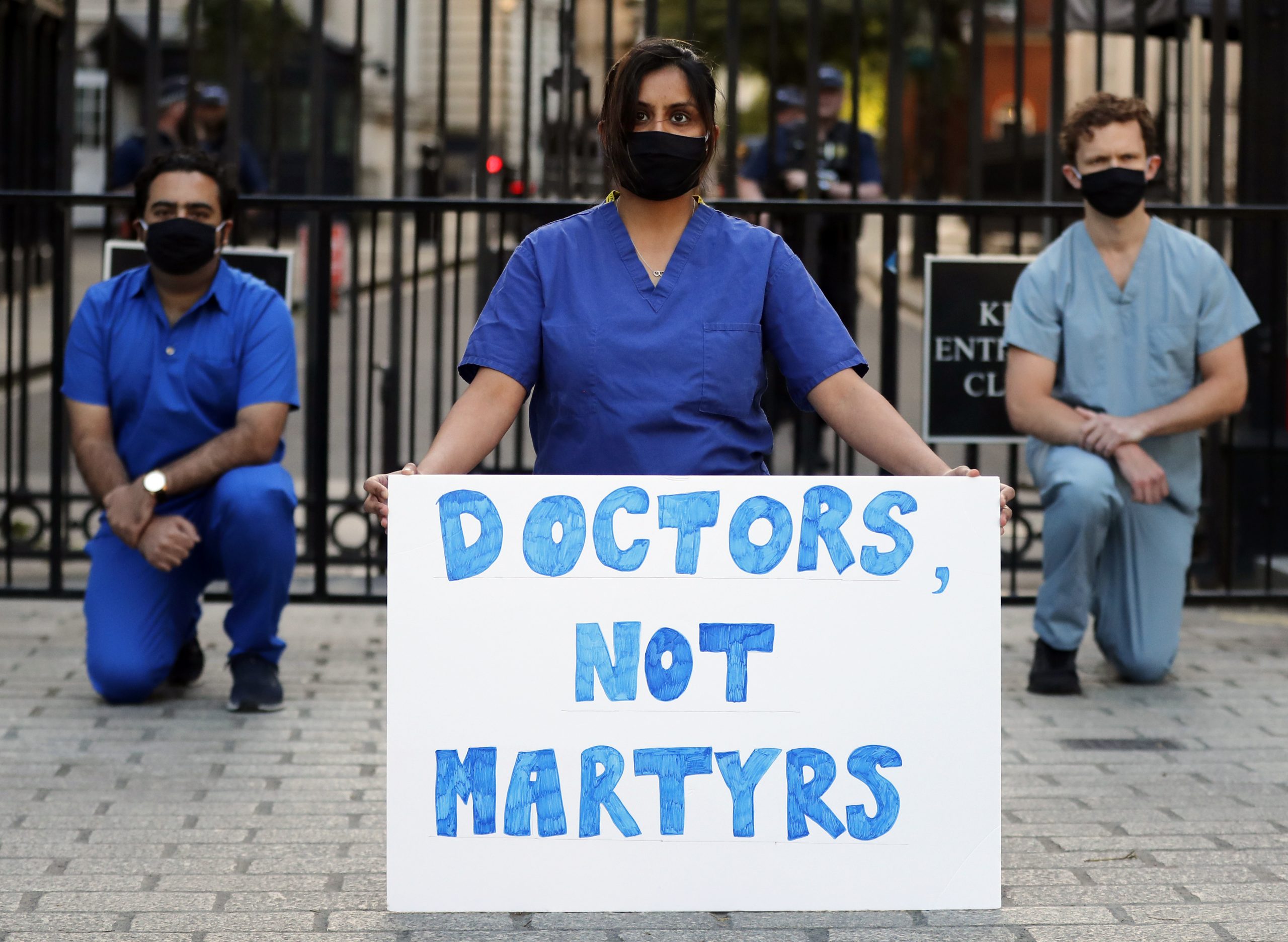
Pressure On Intensive Care
The recognition of how highly skilled and essential nurses truly are has only now begun to dawn on some people, including healthcare leaders.
Working in an ICU requires a unique skill set, which makes it difficult to fully staff the units when they are so busy. Some non-specialists have been re-deployed to critical care from other areas, but all these staff need special training and supervision, causing further stress for the already overstretched ICU nurses.
The standard ratio for ICUs is usually one nurse per critically ill patient. But in response to the pandemic, guidelines have changed so that one nurse can be expected to care for up to four patients depending on the nature of their illness.
This means at any one time, there may not be enough people on hand to safely turn patients in bed, resulting in joint pain and back injury.
The physical strain of wearing PPE for long shifts, which among other things prevents nurses from being able to drink or eat, only adds to the burden for staff.
Ptsd Nursing Care Plans Diagnosis And Nursing Interventions
5 Nursing Care Plans on Post Traumatic Stress Disorder
Its not uncommon for people to suffer from post-traumatic stress disorder after experiencing or witnessing a distressing event. As the name implies, PTSD is a condition and a trauma response to a potentially life-threatening event.
Trauma survivors frequently suffer at first, but with time and good self-care, the vast majority of them are able to recover from their experiences.
PTSD Diagnosis is usually made possible if the symptoms remain for an extended period of time which may persist in months or even years and are usually disruptive to the individuals normal activities.
Recommended Reading: Can Low Blood Sugar Cause Anxiety
Understanding Ptsd: The Role Of Forensic Nurses
View all blog posts under Articles | View all blog posts under Forensic Nursing | View all blog posts under Master of Science in Nursing | View all blog posts under MSN Post-Master’s Certificates
Forensic nurses work closely with victims of violent crimes, providing compassionate medical care while collecting medical evidence to bring perpetrators to justice. Within the scope of their work, forensic nurses must be prepared to identify signs of post-traumatic stress disorder and help victims as they navigate the difficulties that come with the diagnosis.
PTSD is a condition that affects eight million people nationally, according to the U.S. Department of Veterans Affairs and that makes it one of the countrys most prevalent mental health issues. Its symptoms include distressing and unwanted memories, mood changes, sleep disruptions and angry outbursts.
Its normal for people to experience troubling memories, anxious feelings or difficulty sleeping after a traumatic experience. For people with PTSD, these challenges make going through lifes daily routines difficult for months or more.
Understanding PTSD can help forensic nurses as they treat crime victims. Because PTSD can start days, weeks or years after an individual experiences or witnesses a traumatic event, nurses should look to identify signs of PTSD as a result of both recent and past events.