Gray Matter Network Differences Between Probands And Relatives
The pattern of altered anatomic association of the superior temporal cortex in brain networks of probands contrasts with primarily cortical involvement of the frontal lobe in relatives. This represents a significant novel finding. In an investigation using a similar analytic approach, robust gray matter network-based changes in temporal regions were also not seen in relatives of schizophrenia probands . Prior studies performing regional measurements of superior temporal cortex anatomy in unaffected siblings of patients with psychotic disorder also have not found evidence of superior temporal alterations . Thus, alterations in brain network organization involving superior temporal cortex appears to be associated with neuropathological manifestations of psychotic illness, while altered connection of the frontal cortex into brain networks in relatives may be related to familial illness risk.
Comparison Between The Clinical Manifestations In Schizophrenia And In Ad
Alzheimers disease usually begins with a progressive deterioration in memory, and over time additional symptoms accrue that reflect the involvement of other cognitive spheres. The latter symptoms may include aphasia, apraxia, agraphia, and alterations in visuospatial abilities and eventually a disintegration of virtually every cognitive sphere. There are also a few well-documented cases in which uncharacteristically instead of memory loss, the initial manifestation involves a different cerebral cortex-dependent faculty, such as an aphasia, posterior cortical atrophy, or a right parietal syndrome .
Does My Child Have Schizophrenia
Early signs of schizophrenia can be hard to detect because they often overlap with common adolescent behavior. Moreover, these symptoms in people of any age group do not necessarily mean that a person will develop schizophrenia.
These symptoms can be disruptive though, and they may indicate something worrisome is going on, even if it isn’t schizophrenia. If you or your child are experiencing any of these symptoms, you should make an appointment with a healthcare provider.
You May Like: Can You Go To Urgent Care For Panic Attacks
Gray Matter Network Alterations In Relatives
In nonpsychotic first-degree relatives, we observed lower nodal efficiency in the right prefrontal cortex and left hippocampus and pallidum compared with healthy controls, suggesting a reduced use or capacity of these regions for propagating information to other nodes. These results parallel previous findings of lower clustering coefficient values and regional gray matter deficits in right frontal regions , as well as functional and structural abnormalities in the hippocampus , in individuals with familial risk for psychotic disorders. The impaired functional integration between the posterior hippocampus and prefrontal cortex has also been found in individuals at high risk for psychosis .
Hope From Scans Of Schizophrenia In The Brain
Imaging scans of schizophrenia in the brain have helped researchers locate a small area of the brain that may help them predict whether people will develop schizophrenia with 71 percent accuracy for high-risk patients. The study results, which appear in the September 2009 issue of Archives of General Psychiatry, pinpoint the exact area of a part of the brain that shows hyperactivity in schizophrenics.
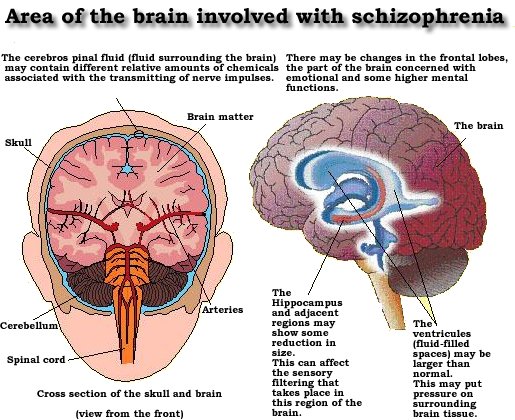
The researchers used high-resolution MRI equipment to show what areas of the brain are affected by schizophrenia. The scientists discovered three areas of the schizophrenic brain that differed from normal brains two areas in the frontal lobes and one very small area of the hippocampus, known as CA1. Weve always known that schizophrenics have a more active hippocampus, the area used for memory and learning, but this study pinpoints the exact spot of hyperactivity in patients with the illness.
This discovery brings new hope and promise to those at risk for developing a schizophrenic brain and for those already suffering from it. Doctors hope that once researchers further develop the findings, that they can use this as a diagnostic marker to predict whether certain high-risk patients will go on to develop full-blown psychosis after prodrome. They also hope to use the CA1 subfield marker in the hippocampus to indicate the efficacy of treatments. For example, a decreased amount of activity in the area could indicate the success of treatment strategies.
Recommended Reading: The Phobia Of Bees
Additional Consultation Needed For Diagnosis
Following any scans or tests, a healthcare professional may make a referral to a mental health expert who has more specialized knowledge on the subject. It is also common for healthcare professionals to speak with the friends and/or family of a person who is showing signs of schizophrenia.
If schizophrenia is diagnosed, then the person with schizophrenia and their support team will work on a treatment plan together.
What Happens To The Body And Brain Of Individuals With Schizophrenia
Richard C. Deth, a professor of Pharmaceutical Science at Northeastern University, provides this answer:
Schizophrenia is a psychiatric disorder in which previously normal cognitive abilities and behaviors becomes disturbed. The most common age of onset is just after reaching adulthood, typically the late-teens to the mid-thirties. It is manifested either by so-called positive symptoms or by negative symptoms, including a marked lack of activity, loss of interest and unresponsiveness.
Although the precise cause of schizophrenia remains unknown, an enormous amount of research has come up with a number of possibilities. Many early theories focused on behavioral or stress-induced events, but more recently, consensus holds that underlying biochemical abnormalities are more likely the cause. Lending great support to this idea is the fact that genetic predisposition may account for 50 percent of the risk of developing schizophrenia. Not surprisingly, these biochemical hypotheses center on dysfunction of the neurotransmitter systems in the brain, which provide for normal cognition and attention. The main theories include the Dopamine Hypothesis, the NMDA Receptor Hypothesis, the Single-carbon Hypothesis and the Membrane Hypothesis. And new research from our laboratory suggests that elements from each of these theories may play a role in schizophrenia.
Don’t Miss: Prodromal Stage Schizophrenia
Subject Demographics And Clinical Characteristics
The demographic and clinical characteristics of the subjects are summarized in Table . There were no significant group differences in sex or age . Eighty-seven patients received medication during the MRI examinations, with the remaining eight patients being treatment naïve. The mean antipsychotic dose was 446.5±341.6 mg/d for the patients with schizophrenia. The mean duration of illness was 121.4±92.8 months. Mean scores on the PANSS positive, negative, and general psychopathology subscales were 17.1±7.9, 20.3±9.1, and 34.1±10.8, respectively.
Table 1 Demographic and clinical characteristics of the participants
Schizophrenia As The Graveyard Of Neuropathologists
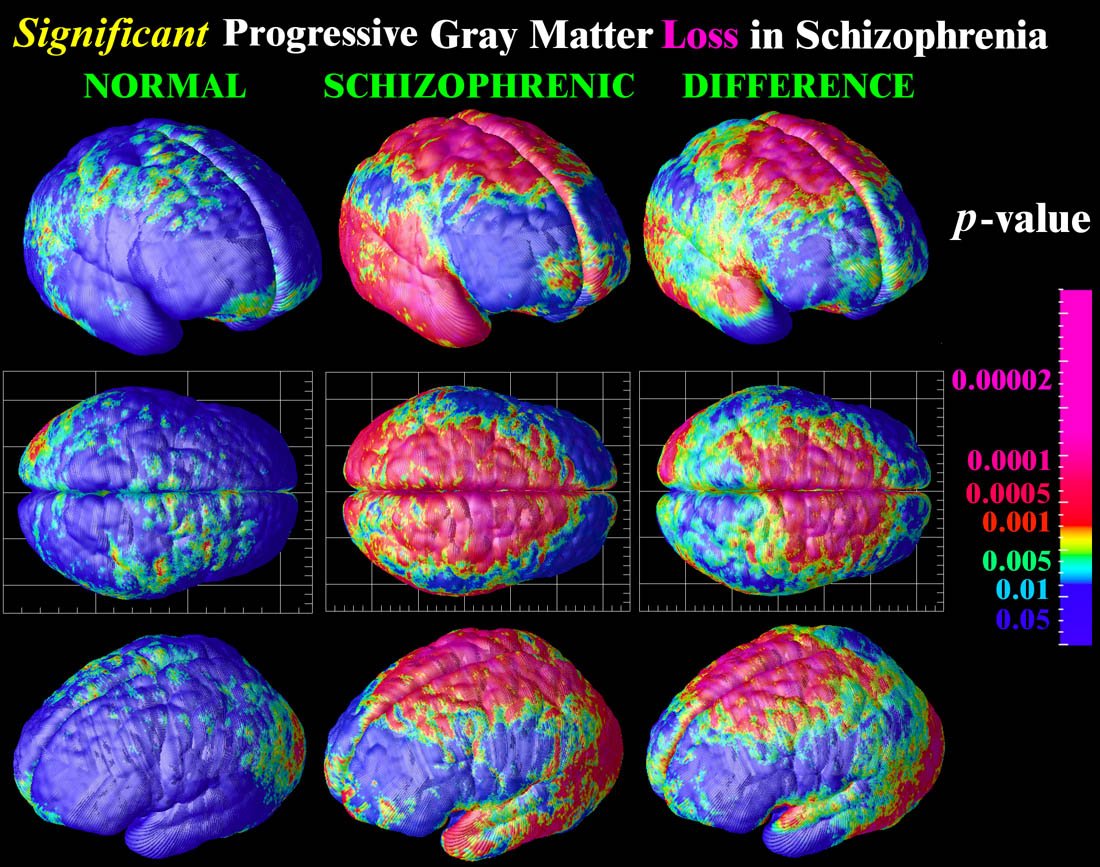
Many believe that schizophrenia and related disorders result from alterations in brain circuits . Yet, this probably correct assumption lacks a concrete factual demonstration hundreds of unverified neuropathological claims non-withstanding and is in stark contrast with the relative wealth of information on the neuropathology of AD because virtually nothing claimed about histopathological observations in schizophrenia has survived efforts at independent verification or corroboration. This justifies Stevens admonition about schizophrenia being the graveyard of neuropathologists , which unfortunately continues to be the case decades since its enunciation. In fact, arguably the only widely accepted, consistent morphological alterations have been found by in vivo imaging, that consist in a reduction in gray matter, enlargement of the ventricles of the brain, and focal alterations in the white matter . This is hardly specific, much less pathognomonic, and is perhaps consistent with the increasingly popular syndromatic as opposed to a unique, or sole disease view of the disorder , which would be consistent with the lack of a truly unique and unanimously agreeable cellular and molecular neuropathology. Be that as it may, it justifies the still vaguely articulated perception that schizophrenia is a disease of the cerebral cortex .
Table 1. A simplified list of selected similarities and key differences between Alzheimers disease and schizophrenia.
You May Like: Feretrophobia Definition
Associations Between The Spatial Distributions Of Gfcd And Gmv
As previously mentioned, increased gFCD were primarily located in subcortical regions, including the basal ganglia and some components of the limbic system and SMA. Decreased gFCD were primarily located in the posterior cortical regions. However, in this study, only decreased GMV was observed. Notably, the aberrant patterns of gFCD and GMV differ between regions. In the caudate, thalami and hippocampus complex , gFCD increased but GMV decreased, while in the posterior cortices, decreased gFCD accompanied decreased GMV. These findings indicated a complex association between gFCD aberrances and GMV changes in schizophrenia. To further investigate whether gFCD correlates with GMV changes, we also performed correlation. In multiple regions, we found that although gFCD and GMV were both affected, there was no statistical correlation between gFCD and GMV either in patients with schizophrenia patients or controls .
Dopamine Signaling And Abnormal Salience Attributions
Dopamine plays a central role in reward-based learning, such that in a particular context, dopamine release is associated with initiation of behaviors that predict reward . Notably, in both prodromal and first-episode patients, the increases in dopamine synthesis are particularly pronounced in parts of the striatum that project to association cortex, including PFC . If increased dopamine synthesis and release began to occur in contexts without prior reward-based contingencies, this could result in a heightened sense of salience of otherwise innocuous stimuli, which could plausibly play a role in the development of ideas of reference and paranoia .
Circuit model of neuronal changes relevant to models of schizophrenia. Excitatory activity of cortical pyramidal neurons is thought to be reduced in schizophrenia, most likely due to NMDA receptor hypofunction. Because of interactions with inhibitory, GABAergic interneurons , decreased excitatory input to neurons in the mesencephalon would lead to increased dopamine activity in the striatum and decreased dopamine activity in the cortex . Reprinted by permission from the American Society of Clinical Investigation: Journal of Clinical Investigation , copyright 2009.
Read Also: Does Dehydration Cause Panic Attacks
Schizophrenia: Early Warning Signs
Early detection and treatment of conditions such as heart disease and cancer have improved survival rates and quality of life for people who suffer from these conditions. A new approach involves identifying people who show minor symptoms of psychosis, such as unusual thought content, paranoia, odd communication, delusions, problems at school or work, and a decline in social functioningwhich are coined prodromal symptomsand following these individuals over time to determine which of them develop a psychotic disorder and which factors best predict such a disorder. A number of factors have been identified that predict a greater likelihood that prodromal individuals will develop a psychotic disorder: genetic risk , recent deterioration in functioning, high levels of unusual thought content, high levels of suspicion or paranoia, poor social functioning, and a history of substance abuse . Further research will enable a more accurate prediction of those at greatest risk for developing schizophrenia, and thus to whom early intervention efforts should be directed.
DIG DEEPER
Brain And Body Risk Factors
Developmental theories of schizophrenia suggest that something goes wrong when the brain is developing. Brain development, from the earliest stage of fetal development, the early years of life and through adolescence, is an extremely complicated process. Millions of neurons are formed, migrate to different regions of the forming brain, and specialize to perform different functions.
The something that goes wrong might be a viral infection, a hormonal imbalance, an error in genetic encoding, a nutritional stress, or something else. The common element in all developmental theories is that the causal event occurs during the brains development.
Even though these potential causes may be rooted in very early development, symptoms of schizophrenia typically emerge in late adolescence or early adulthood.
Recommended Reading: Anya Shumilina
Studies Of Relatives And Others At Risk
sMRI studies of the MTL have been the focus of most attention in people at risk. Early ROI studies tended to examine the amygdala and hippocampus together and consistently found reductions in relatives compared with controls, but most relatives did not have volume reductions to pathological levels., The balance of the evidence was for hippocampal differences in particular, although there were some notable and quite large negative studies. A comprehensive review concluded that reduced hippocampi were likely to be a vulnerability marker for schizophrenia. This view has recently been supported by a systematic review and meta-analysis of studies of relatives that finds hippocampal reductions in relatives, with an effect size of about 0.3, and additional differences between relatives and patients.
Despite the small number of studies, there are already replicated computational voxel-based morphometry studies in the relatives of patients with schizophrenia vs bipolar disorder. Both Job et al and Diwadkar et al found reduced gray matter in PFC in relatives at high risk for schizophrenia. Similarly, both McIntosh et al and McDonald et al have reported reductions in gray matter density in prefrontal regions and thalamus in schizophrenia as distinct from no reductions in gray matter in these regions in bipolar disorder. Reductions in the thalamus have been reported as a measure of genetic liability to psychosis in general.,
How Is Schizophrenia Diagnosed
To diagnose this disease, your healthcare provider will ask about your medical history and symptoms. You may also have a physical exam. You may also have lab tests to rule out other conditions.
Mental health care professionals diagnose and treat this illness. They often interview family members. This helps the healthcare team get a complete picture of the symptoms.
Read Also: Feretaphobia
Gm Volume Alterations In Subjects With Schizophrenia
In this study, differences in brain structure between the healthy persons and the more favorable subgroups of patients could not be detected . In the same way, the differences between the more favorable and the more unfavorable subgroups of patients were not statistically remarkable .
In addition to the whole group, the differences between the unfavorable subgroups of patients and the healthy controls reached the level of significance. In the cases of patients who belonged to either or both of the subgroups with more unfavorable natures , there were verified notable brain structural differences compared to the healthy controls. Most of the relevant areas were revealed in the analysis between cluster S and the healthy controls.
Schizophrenia Group vs. Healthy Controls
The whole mixed group of patients with schizophrenia was measured to have lower GM volumes in the left insular cortex and left inferior frontal gyrus compared to the healthy controls .
Table 2. Significant volumetric clusters of gray matter volume deficits in the group of patients with schizophrenia compared to the healthy controls.
Deficit-Syndrome vs. Healthy Controls
The deficit group showed lower cortical GM volumes in the bilateral perisylvian area, in the right orbitofrontal cortex and in the inferior and polar areas of the left frontal cortex compared to the normal controls.
S-Cluster vs. Healthy Controls
Extraction Of Brain Networks
We followed the methodology proposed by Tijms et al. to extract individual structural morphology brain networks, which is a completely automated and data-driven method. This approach takes both local morphology and folding structure of the cortex into account, improving accuracy in the characterization of morphological network topology . In brief, the method defines network nodes as regions of interest corresponding to 3×3×3mm3 voxel cubes, and their connection refers to edges, indicating statistically similar gray matter morphology of two cubes as determined with correlation coefficients. Weighted graphs are constructed after determining a threshold for each individual graph with a permutation-based method to ensure a significant similarity for all individuals . Because network properties can vary with network size , we normalized gray matter networks using the methodology proposed by Batalle et al. based on the Automated Anatomical Labeling parcellation template .
Also Check: Blacking Out During Panic Attack
Challenges In Diagnosing Schizophrenia
Psychiatric symptoms exist on continua from normal to pathological, meaning the threshold for diagnosis of schizophrenia in clinical practice can be challenging. The clinical diagnosis of schizophrenia relies heavily on the positive symptoms associated with a prolonged psychotic episode. However, a relatively high percentage of the general population report delusional experiences or hallucinations in their lifetime,,, but for most people these are transient. Psychotic symptoms are also not specific to a particular mental disorder. The clinical efficacy of antipsychotic drugs is heavily correlated with their ability to block subcortical dopamine D2 receptors, , suggesting dopamine signalling is important. In spite of this, no consistent relationship between D2 receptors and the pathophysiology of schizophrenia has emerged, . In contrast, the clinical evidence points towards presynaptic dopamine dysfunction as a mediator of psychosis in schizophrenia.
What Are The Symptoms Of Schizophrenia
Each person may feel symptoms differently. These are the most common symptoms:
-
False beliefs not based on reality
-
Seeing, hearing, smelling, or feeling things that are not real
-
Disorganized speech and behavior
-
Feeling like someone or something is out to get them
-
Withdrawal from others
-
Inflated self worth
These symptoms can make it very hard to function in the world and take care of yourself. People with this illness are usually not violent.
The symptoms of schizophrenia may look like other problems or mental health conditions. Always see your healthcare provider for a diagnosis.
Read Also: Can Low Blood Sugar Cause Anxiety
Neurodevelopment Medial Prefrontal Cortex And Errors In Source Monitoring
Brain dysconnectivity in schizophrenia is thought to derive primarily from deficits in dendritic spines that arise during development , though axonal pathology may also play a role . Such deficits are likely to be present at least in part in some cases from birth, resulting from an interplay of genetic factors and obstetric complications , but may progress beyond a threshold critical for expression of psychotic symptoms as a function of normal neuromaturational events during adolescence . In other cases, dysconnectivity may emerge during late adolescence and early adulthood as a consequence of overly aggressive synaptic pruning and/or other aberrant processes, such as elevated cortisol leading to dendritic atrophy . The contributions of early and later brain developmental processes to psychosis risk are not mutually exclusive, and both sets of processes may be operative in some cases .
Developmental trajectories of cortical synaptic connectivity, including a number of trajectories in which connectivity is reduced below a hypothetical threshold sufficient for expression of psychotic symptoms.
Cortical surface maps showing regions in which converters to psychosis had significantly greater progressive loss of gray matter thickness compared with non-converters and controls Cortical surface maps showing regions in which higher levels of unusual thought content at baseline predicted a steeper rate of gray matter thinning among converters .