Do You Feel Sleep Deprived
Take our 2-minute Sleep Deprivation and Depression quizzes to see if you simply aren’t getting enough sleep or if you may benefit from further diagnosis and treatment.
Take Sleep Deprivation QuizTake Depression Quiz
Sleep deprivation weakens the prefrontal cortexs ability to control the amygdala , making it difficult to process and cope with emotions. When the brain is deprived of adequate sleep, it also struggles to concentrate and regulate growth and appetite.
Sleep deprivation can have a profound effect on both the emotional and cognitive functioning of the brain. This results in bad moods, negative thinking, decreased empathy, and poor impulse control.
The good news is that sleep deprivation can be treated, and getting on a regular sleep cycle can alleviate the above symptoms.
Depression And Sleep: Understanding The Connection
Health Risks of Poor SleepAge-Related Depression, Mood and StressAging and Sleep
Depression and sleep problems are closely linked. People with, for example, may have a tenfold higher risk of developing depression thanpeople who get a good nights sleep. And among people with depression, 75percent have trouble falling asleep or staying asleep.
Which comes first? Either one can be the starting point, says Johns Hopkins sleep researcher Patrick H. Finan, Ph.D. Poor sleep may create difficulties regulating emotions that, in turn, may leave you more vulnerable to depression in the futuremonths or even years from now. And depression itself is associated with sleep difficulties such as shortening the amount of restorative slow-wave sleep a person gets each night.
If you have , daily stressessuch as financial worries, an argument with your spouse, or a jam-packed evening commutecould also lead to more nighttime wake-ups and more trouble getting back to sleep than someone without depression would experience.
Understanding the relationship between insomnia and depression can help you spot risks early, get the right help, and recover more fully if you are experiencing both. Youll feel healthy, well-rested, and able to enjoy life again. Heres what you need to know about depression and sleep:
Distress And Quality Of Life
Disturbed sleep is a very distressing symptom which has huge impact on quality of life in depressed patients. We surveyed the views of patients with depression about their symptoms and associated sleep difficulties. In this study, 2800 members of Depression Alliance, a UK-based charity for people with depression, were sent a postal questionnaire. Respondents were asked if, when they are depressed, they suffer from sleep difficulties .
What Is The Treatment For Depression
-
Talk therapy or psychotherapy .
-
Lifestyle changes .
-
Complementary therapies .
-
One or more prescription medicines.
It is not uncommon to use more than one type of treatment. For example, a person may establish a regular exercise routine, start seeing a therapist, and begin taking antidepressant medicine.
What Are The Reasons For Depression

It is not well-known what causes depression. Similarly as with numerous mental issues, an assortment of variables might be included, for example:
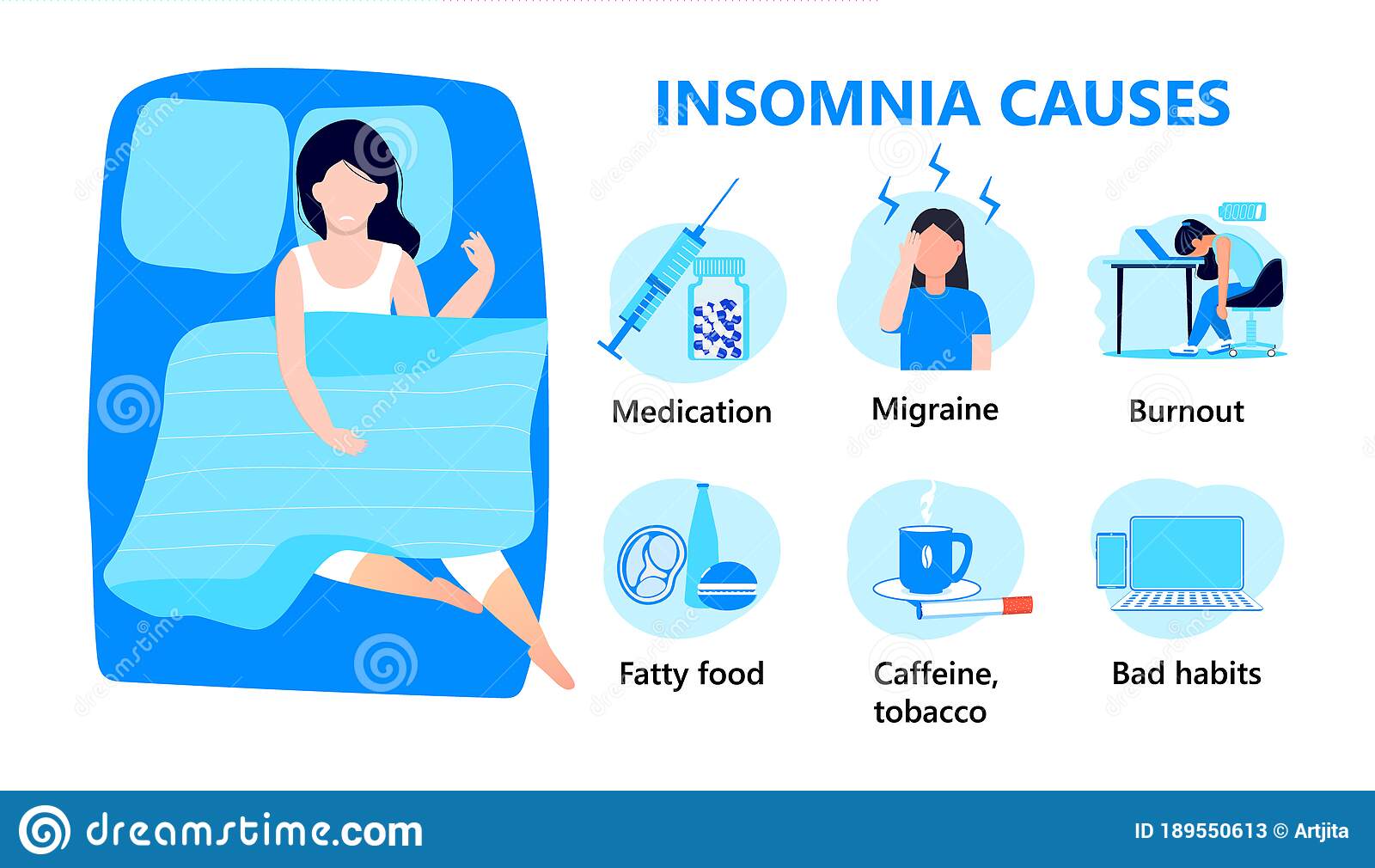
- Insomnia can cause depression. Trouble resting is some of the time is the principal manifestation of depression. 15 to 20 percent of individuals determined to have a sleeping disorder will create depression.
- Biological differences can create depression. People with discouragement seem to have physical changes in their brains. The centrality of these progressions is still dubious, yet might, in the long run, pinpoint causes.
- Brain chemistry can cause depression. Neurotransmitters are normally happening mind chemicals that probably assume a part in misery. Late research shows that adjustments in the capacity and impact of these neurotransmitters and how they collaborate with neurocircuits included in keeping up disposition soundness might assume a critical part of melancholy and its treatment.
- Hormone changes can reason to depression. Changes in the bodys parity of hormones might be incorporated in bringing on or activating despondency. Hormone changes can come about with pregnancy and amid the weeks or months after conveyance and from thyroid issues, menopause or various conditions.
- Inherited characteristics can contribute to depression. Depression is more normal in individuals whose blood relatives have the same condition; Scientists are attempting to discover qualities that might be included in creating sadness.
What Are The Types Of Depressive Disorders
Significant feelings of sadness or a loss of interest in their normal daily activities are common in all depressive disorders. Specific forms of depression vary based on the severity of symptoms and the situation in which they develop.
The most well-known type is major depressive disorder, and it is marked by symptoms that affect a person virtually every day for an extended period of time. It commonly involves sleep disruptions.
Persistent depressive disorder, also called dysthymia or chronic depression, may involve fewer symptoms than major depression, but symptoms last for at least two years and any symptom-free period lasts no longer than two months.
Other types of depression, such as premenstrual dysphoric disorder and seasonal affective disorder tend to come and go over shorter periods but can also involve significant sleeping problems.
Depression Symptoms To Watch For
While severe sadness is the most well-known symptom of depression, knowing how to recognize other signs can help head off a future depressive episode.
If you’re one of the 20 million people in America with depression, you know that it’s not a condition to be taken lightly. It’s important to manage symptoms of depression with therapy and medication as prescribed by your doctor, both to feel better now and to reduce the risk of a depressive episode in the future.
One of the best ways to minimize the physical and emotional damage of an episode of depression is to recognize depression early and take action which can mean getting back on track with treatment or talking to your doctor about whether your treatment plan needs to be reviewed and revised. But not all symptoms of depression are easy to identify, and the early signs can be different for everyone. Here are some common symptoms you should look for.
Insomnia And Risk Of Developing Depression
While some may categorize insomnia and other sleep disorders as symptoms of a depressive disorder, research has proven that they may actually be antecedents to depressive episodessuggesting that depression could actually be categorized as a symptom of insomnia. For younger adults along with middle-aged individuals, insomnia was found to lead to a two to four-fold increased risk for having a relapsed depressive episode later in life.
In addition, researchers have posited that complaints of episodes of insomnia almost every night for two weeks or more could be a useful indicator to predict a major depression episode for those who have struggled with depression in the past. The link is not only reserved for those who have struggled with past depression, however. In fact, research studies show that 14% of individuals who struggled with insomnia at one date developed new major depression one year later, suggesting that for some individuals, insomnia can lead to new depressive disorders and not simply exacerbate old ones.
Sleep Disorders and Mood Changes
The Health Risks Associated With Depression And Sleep Disturbances
Depression and sleep disturbances can take a toll on your physical health if left untreated. One 2010 study found that lack of sleep was associated with a higher risk of early death. Lack of sleep increases the risk of heart disease and failure, heart attacks, high blood pressure, stroke, diabetes, and obesity.
Depression can constrict blood vessels, which may increase your risk of heart disease. People with depression may experience a weakened immune system, aches and pains, and fatigue.
What Is The Link Between Insomnia And Depression
A failure to rest is one of the key indications of clinical depression. Another sign of clinical depression is over dozing or oversleeping.
Having a rest issue does not in itself cause sadness, but rather the absence of rest plays a part. The lack of rest created by another curable disease or by individual issues can aggravate despondency/depression. A failure to rest that keeps going over a drawn out stretch of time is likewise an essential piece of information that somebody might be discouraged.
Coping With Depression And Insomnia
When battling both depression and insomnia or any mix of the two, the road to recovery can be long and difficult. With the right approach and treatment methods, you can identify the root cause of your issue and take the necessary steps to relieve symptoms.
Try to be in-tune with your feelings and triggers. Combat feelings of sadness by incorporating exercise into your daily routine. This will also promote better sleep. A well-rested mind is better equipped to deal with depression symptoms.
Dont be afraid to ask for help. Depression can be a very isolating condition and is often accompanied by feelings of helplessness and hopelessness. Its important to have a support group around you that understands your condition and offers positive tools and resources. The same can be said for overcoming insomnia. A partner who supports your sleep schedule and nightly routine are crucial. Together, you can create a calming sleep environment complete with dim lighting, soothing sounds, and minimal distractions.
If your feelings of depression or overwhelming exhaustion due to insomnia leave you feeling hopeless, its important to recognize suicidal thoughts and seek help immediately.
Treating Pain And Depression
Although the treatment of pain and depression is beyond the scope of this article, there are many ways that patients can help themselves deal with depressive symptoms associated with chronic pain. Table 3 describes some self-directed approaches. For instance, natural lighting, especially in the winter, may help increase serotonin levels and improve mood. To increase light exposure, patients can walk briefly outside in the morning, sit next to a bright, sunny window, and use full-spectrum light bulbs indoors. Increasing activity levels is another option. Although often difficult to initiate, physical exercise, particularly aerobic exercise, is one of the most effective treatments for depression. It also is beneficial to avoid other chemical depressants, such as alcohol,62 and to set up a routine, so that it becomes habit to get things done rather than to become inactive due to depressive symptoms.
Aside from self-help, there are a wide variety of other treatments available for depression and chronic pain. Typically, the first treatment used for musculoskeletal injury is primary rehabilitation, which helps control pain and encourages typical healing. Over-the-counter analgesics, muscle relaxants/opioids in rare cases, and physical agents such as ultrasound, heat, cold, and electrical stimulation all are examples of primary rehabilitation treatment.
How Are Depression And Insomnia Related

Medically Reviewed By: Tonia Cassaday
Both depression and insomnia are common disorders that cause people some disturbance worldwide. When dealing with either of these issues, the person can have difficulty maintaining a good quality of life. Scientists estimate that 40% of Americans will struggle with insomnia at one point in their life, while an estimated 17.3 million U.S. adults will deal with the symptoms of a major depression episode at least once per year. Depression and insomnia are often linked as interrelated disorders, and they are often related in a variety of ways. In fact, some scientists have gone so far as to suggest that medical practitioners should be wary of diagnosing depression without evidence of sleep complaints by the individual. So, how are depression and insomnia related?
Dont Let Depression Or Insomnia Rule Your Life
There is hope when it comes to treating and overcoming both depression and insomnia. Whether youre struggling most with feelings of sadness and frustration or, instead, extreme exhaustion and irritability caused by insomnia, help is available. The first step is recognizing and being honest about your symptoms. Once you get over this hurdle, you can start on the road to recovery.
At Somnus Therapy, were dedicated to giving you your life back. Through a mix of therapies, activities, and resources, we help treat sleep disorders and insomnia from the comfort of your home. This online program is perfect for those dealing with insomnia caused by depression or those who fear their depression is creating a sleep disturbance.
Find out more about how Somnus Therapy works by and always be sure to seek professional help if your depression symptoms worsen or you experience thoughts of hurting yourself or others.
Sleep Therapy At Home
Our guided insomnia treatment program has helped over 2,000 users sleep better, faster & longer – all from the comfort of their own home.
Menopause Depression And Sleep
For those already struggling with depression during the menopause transition, an effective intervention may lie in a better nights sleep.
People with insomnia are twice as likely to develop depression compared to those without insomnia.
Hadine Joffe, MD, MSc, director of the Womens Hormones and Aging Research Program in Brighams Department of Psychiatry, is working to build a better understanding of the biological mechanisms behind depression in women.
In a study published in the Journal of Clinical Endocrinology and Metabolism, Dr. Joffe and her team detailed how hot flashes, hormones, and sleep affected women with menopause-associated depression. Seventy-two peri- and post-menopausal women experiencing depression, hot flashes, and sleep disturbance were randomized to receive estradiol , zolpidem or placebo for eight weeks.
Dr. Joffe observed that for peri- and post-menopausal women, depression symptoms improved when their sleep quality improved, regardless of what treatment they were given.
These particular results show that targeting insomnia in peri- and post-menopausal women may be critical in the overall management of depression, said Dr. Joffe.
Charles A. Czeisler, MD, PhD, Chief of the Division of Sleep and Circadian Disorders at the Brigham, explains the impact of sleep on brain function and physical health.
Charles A. Czeisler, MD, PhD, is Chief of the Division of Sleep and Circadian Disorders at Brigham and Women’s Hospital .
Talk To Your Physician
Difficulty sleeping may stem from an underlying medical condition, such as obstructive sleep apnea. Restless leg syndrome and bruxism can also interfere with sleep. These medical issues may cause sleep problems that worsen or cause depression.
Its important to talk to your physician about any sleep problems or depressive symptoms youre experiencing. Your physician can assess whether you have underlying health issues contributing to your conditions.
Depression-Like Symptoms That Aren’t Depression
Depression And Insomnia Should Be Treated Individually
A common belief that insomnia is a secondary symptom of depression when they co-occur is not supported by scientific evidence, and doctors should direct targeted diagnostic and treatment attention to both disorders, according to a narrative review published by the Medical Journal of Australia.
Up to 90% of patients with mood disorders also report difficulties initiating and/or maintaining sleep, and about 2050% of patients with insomnia disorder report symptoms of depression, say the authors of the review, led by Dr. Alexander Sweetman, a Research Associate at the Adelaide Institute for Sleep Health at Flinders University.
“The co-occurrence of depression and insomnia is associated with reduced quality of life, greater overall morbidity, and increased health care use, compared with either depression or insomnia alone,” Dr. Sweetman and colleagues write.
“Therefore, it is critical to consider diagnostic and management approaches for patients with co-occurring depression and insomnia to improve patient outcomes and reduce health care costs.
“Depression is commonly conceptualized as the primary disorder, and the insomnia as a secondary symptom. This is evidenced by clinicians prioritizing the management of depression over insomnia, and an expectation that insomnia symptoms will abate when depression is successfully managed.”
The evidence suggests, however, that insomnia and depression should be treated as separate disorders, and the authors detailed six areas of evidence:
How Symptoms Of Depression Impact Sleep
Untreated depression can lead to overwhelming sadness, which can affect your ability to sleep. During the night, your mind may ruminate about things that are contributing to negative emotions including sadness, despair and hopelessness.
While you are lying in bed tossing and turning, the bad feelings you are having can seem much more impossible to deal with. And the more you focus on your uncomfortable emotions, the harder it is to sleep.
Get Help For Both Depression And Sleep
If you have insomnia and depression, dont assume that medical treatment for one will automatically cure the other. Treatments for depression, such as selective serotonin reuptake inhibitors and other medications, may improve your mood and outlook, but they may not be enough to improve your sleep.
Theres some evidence that lingering sleep problems in people undergoing depression treatment increase the risk of a slide back into depression. The good news: Theres also some early evidence that CBT-I , along with depression treatment, improves sleep in people with depression and may increase the chances of a remission of depression.
Poor Quality Sleep Reduces Resilience
In a recent Johns Hopkins study, healthy women and men whose sleep wasinterrupted throughout the night had a 31 percent reduction in positivemoods the next day. Sleep interruptions interfere with deep, restorativeslow-wave sleep, explains lead researcher Patrick Finan, Ph.D. Ongoing insomnia could increase a persons risk of depression, he says, byweakening their emotional resiliencethe buffer of positive emotions thathelps people deal with stress and challenges of life.
Take Sleep Problems Seriously
You should tell your doctor if you:
- have trouble falling or staying asleep
- feel tired during the day
- have physical pain, discomfort or other complaints that prevent you from getting a good nights sleep
Treatments such as cognitive behavioral therapy for insomnia and continuous positive airway pressure devices for apnea can restore good sleep, helping you sidestep related conditions like depression.
The Link Between Sleep Disturbances And Depression
Approximately 80% of people with depression experience sleep disturbances. While some have trouble falling asleep, others have difficulty staying asleep. And some find themselves sleeping too much.
Both depression and insomnia involve chemicals in the brain. Changes in neurotransmitters and hormonal imbalances may affect both sleep and mood.
For many years, researchers studied which came first: depression or insomnia. It was clear that the two issues often go hand-in-hand and exacerbate one another.
Studies show that sleep disturbances often occur before depression begins. Experiencing insomnia prior to feeling depressed may increase the severity of depression.
The American Academy of Sleep Medicine now encourages treatment providers to pay close attention to whether insomnia needs to be identified as a separate condition as opposed to viewing it as a symptom of depression only.
Getting Back On Track
If oversleeping is a symptom of depression, its most important to see a healthcare provider for treatment of that depression. And even if someone is being treated for depression, the sleep difficulties can be residual. Sleep can remain a struggle because its developed a life of its own and become very habitual, she says.
Dr. Drerup does have a few suggestions on how you can avoid falling into bad sleep habits that could exacerbate the sleep situation. These techniques can make a huge difference for people when they implement behavioral changes like this because the mood symptoms arent impairing them.
If people can get out of bed and get a more consistent start to their day, it can make their day better, Dr. Drerup says. They feel like they can be more productive and get more accomplished. And it can help improve their mood and allow them to make other changes over time that helps increase more pleasurable activities and engaging with people instead of the oversleeping and avoidance of interactions.
Hands off the snooze button
This may not be a popular idea given how much its a ritual for so many of us. But Dr. Drerup points out that repeatedly hitting the snooze button doesnt really help you. When you hit the snooze button and you doze for those short seven or eight minute increments, youre getting brief, fragmented sleep periods. You may think youre gradually becoming more alert but really youre developing sleep inertia and your body wants to stay asleep.
Which Types Of Antidepressants Can Help With Sleep
Your doctor may prescribe one of the following antidepressants that can also help you sleep:
- An SSRI such as , ,  ,  , and  can be effective for treating depression but may take several weeks or longer to become effective. At the beginning, they may also cause or worsen insomnia, for which your doctor may prescribe a separate sleeping medication on a short-term basis. Other antidepressant medicines that affect serotonin through multiple serotonin receptors include  and  .
- SNRIs such as  , desvenlafaxine succinate ,  ,  , or Â
- Sedating antidepressants such as  . The antidepressant  is not widely used to treat depression but because it can cause drowsiness it is often paired as a sleep aid.
Insomnia As A Subsequent Symptom
According to Harvard Health, 69% of people with insomnia also struggled with depression later on. In another study, 21% of individuals reported that they struggled with a combination of hypersomnia and insomnia. These two studies suggest that depressive episodes may cause insomnia or hypersomnia. Issues with sleep due to depression can happen in a variety of ways, including changes to sleep regulation processes or side effects of prescription medication. This, in turn, may exacerbate symptoms of depression, but experts in a U.K. study that depressive disorders without insomnia or other sleep disorders are increasingly rare.
Behavioral Chronotherapy And Chronopharmacology
Another very relevant aspect of chronomedicine is Chronopharmacology, the timing of drug intake. Antidepressants in particular involve a number of neurotransmitters that are acting directly on the SCN or in circuits, which are regulated by the timekeeping system, for example the SCN has serotonin receptors and lithium is known to prolong the circadian period.
Unfortunately, up to now no data are available how frequent chronotherapeutic approaches are used for the treatment of circadian and other disordersthis is in contrast to prescribed medications and psychotherapeutic treatments, where usually sales figures or statistics derived from national health care systems can give at least a rough indication how frequently a certain intervention is applied. This is in part due to the fact that for example an intervention like sleep deprivation or light therapy in a depressed patient applied in a hospital will produce no tangible costs to figure in a statisticthus apart from enhancing awareness for circadian/chronobiological disorders it will also be a challenge to collect data on the specific treatment modalities in clinical care to get an impression of their effectiveness in routine clinical care.
Best Treatment For Co
Treatment for depression nearly always includes a combination approach of antidepressant therapy and psychotherapy, namely cognitive behavioral therapy . However, it has been observed that those with a sleep disturbance like insomnia may not be responsive to CBT long-term. This is because the problematic sleep patterns may endure, leading to relapse back to depression even after successful CBT therapeutic outcomes. In other words, insomnia undermines the CBT treatment success.
That said, there is a form of CBT that is tailored for treating individuals with insomnia. CBT-I is a short-term, goal-directed type of psychotherapy that involves 4-6 sessions. CBT-I may begin with the individual undergoing a sleep study to determine the sleep rhythm and sleep dysfunction present. During the CBT-I therapy, clients are asked to keep a sleep diary that helps them track specific triggers, such as racing thoughts, and to acquire coping skills that help regulate these disruptive thoughts and feelings.
Those who have an enduring issue with sleep disturbance may benefit from a combination of drug therapies, including antidepressants plus a sleep aid from either the benzodiazepine family of drugs or hypnotics like Ambien. Holistic treatments can also provide some measure of relief from the sleep problems. These might include:
Create Time To Decompress Before Bed
This may be especially important if rumination is causing insomnia. O’Neill says this can be any calming bedtime ritual that primes the body to expect sleep, such as dimming the lights and reading a book, or taking a bath.
Make sure to avoid the blue light of electronics, or stressful activities like watching TV or reading the news, as this can have a stimulating effect.
Differentiating Treatment For Insomnia And Depression In Chronic Pain
As noted, one symptom of depression is insomnia. However, that does not mean that insomnia is a secondary symptom of depression in patients with chronic pain. Insomnia can occur without major depression in patients with chronic musculoskeletal pain.8 Patients with chronic pain and concurrent major depression and insomnia report the highest levels of pain-related impairment, but insomnia in the absence of major depression is also associated with increased pain and distress, noted Wilson et al.8 In a chronic musculoskeletal disorder population, patients classified as having moderate and severe clinical insomnia do not always score high on depression measures.9 These findings further support the notion that insomnia is not a secondary symptom of depression. Thus, it is imperative to differentiate the treatment of insomnia from that of depression treatment for patients with chronic pain.