What Is The Difference Between Schizophrenia And Multiple Personality Disorder
Multiple personality disorder is not something a person is born with.
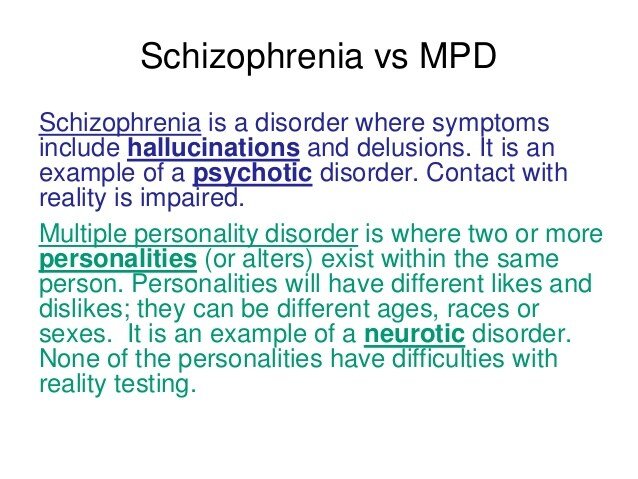
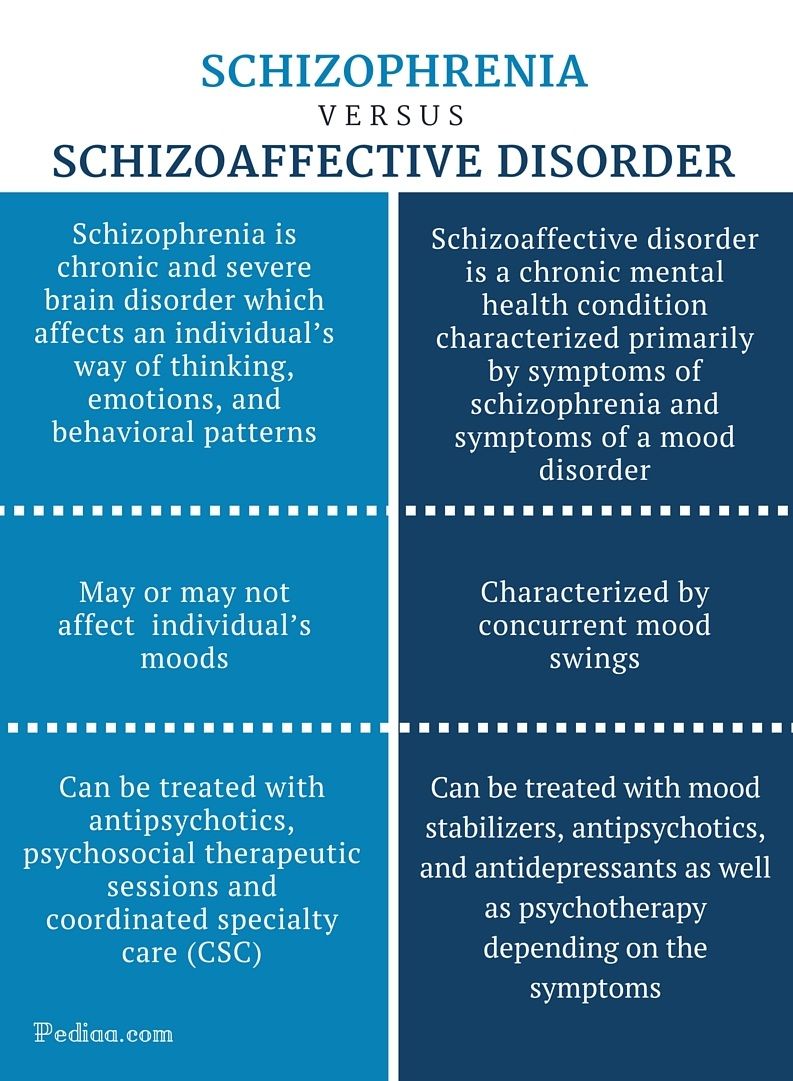
Often, and multiple personality disorder are confused, and some people believe they are the same. In reality, they are two distinctly different disorders. Schizophrenia is a disorder that some people are born with — it may be inherited, but symptoms don’t usually develop for many years. In men, symptoms often develop in late adolescence or the early 20s; for women, symptoms often appear in the 20s or 30s. Sometimes, symptoms do develop during childhood, but this is rare.
Individuals with multiple personality disorder tend to “lose” time.
When a person has schizophrenia, he experiences and , seeing things that aren’t there and believing things that are clearly not true. For example, he may see demons sitting next to him at dinner or believe he is the son of God. A person with this condition also suffers from disordered thinking, decreased attention span, and problems with focusing. Typically, those with this disorder withdraw socially. It’s also common for those with this condition to appear expressionless and lose their ability to initiate and carry out plans.
Halluncinations, auditory delusions and social withdrawal are symptoms of schizophrenia. People who suffer from either schizophrenia or multiple personality disorder have an increased risk of attempting or committing suicide.
Whats The Difference Between Dissociative Identity Disorder And Schizophrenia
Sometimes, people confuse dissociative identity disorder, formerly known as multiple personality disorder, and schizophrenia. Schizophrenia does mean “split mind,” but the name was meant to describe the ‘split’ from reality that you experience during an episode of psychosis, as well as changes in thoughts, emotions, and other functions. Dissociative identity disorder, on the other hand, does cause a split or fragmented understanding of a person’s sense of themselves.
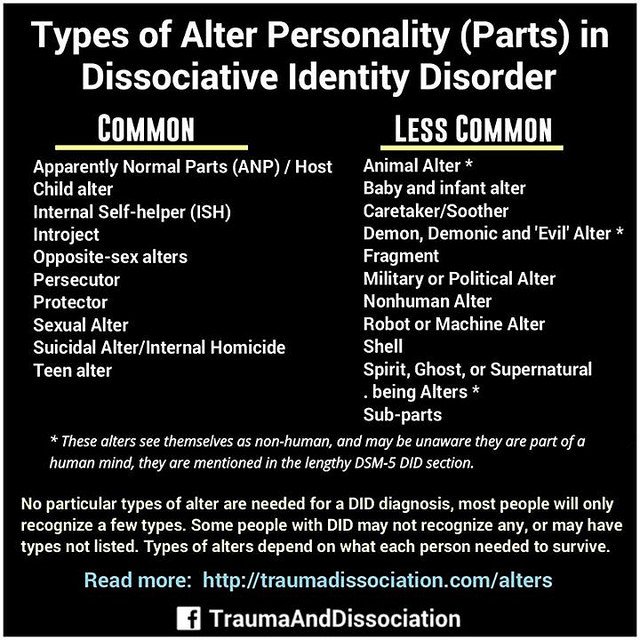
Dissociative identity disorder is really more about fragmented identities than many different personalities that develop on their own. Most people see different parts of their being as part of the whole person. For people who experience DID, identity fragments may have very different characteristics, including their own history, identity, and mannerisms. A key part of DID is dissociation—feeling detached to the world around you. People who experience DID may have many unexplainable gaps in their memory, forget information they’re already learned, or have difficulties recalling things they’ve said or done. Unlike portrayals of DID on TV or in movies, DID may not be obvious to others, and it can take a lot of time to come to the diagnosis.
Where can I learn more?
About the author
#1 Myth: Schizophrenia Means You Have A Split Personality
Reality: “This is a classic myth,” Dr. Rego says. A split personality, also called a Dissociative Identity Disorder or a Multiple Personality Disorder, is extraordinarily rare, he explains. It is quite distinct from schizophrenia, he says. “Schizophrenia is a thought disorder,” he explains, “The myth likely stems from the fact that in schizophrenia there is a breakdown, or split, between thoughts, emotions, and behavior.”
This split results in the person confusing reality and fantasy, Dr. Rego explains. “The person may experience delusions and hallucinations, and emotions may become blunted or inappropriate,” he explains. When most people think of schizophrenia, they think of someone who is seeing things and hearing voices, Dr. Rego points out. “These are what are called positive symptoms, but people with schizophrenia have negative symptoms, too,” he says. Among the common negative symptoms are low motivation, difficulty forming social connections, and a flat, blunted affect, Dr. Rego says. A lack of pleasure in everyday activities, rarely speaking, and difficulty paying attention are also symptoms, according to the American Psychological Association.
Early Detection Of Psychotic Disorders
In clinical samples, the early detection of psychoses mainly follows an indicated preventive approach. Currently, a CHR state is alternatively defined by two complementary approaches : The ultra-high risk approach, developed to identify persons with high likelihood of transition to psychosis within the next 12 months, and the basic symptom approach, developed to detect beginning psychosis as early as possible.
The basic symptom criteria include “cognitive disturbances” and the “cognitive-perceptive basic symptoms” . Of these, the latter lacked sufficient meta-analytical evidence to be already recommended for clinical practice . Contrary to the trait character of schizotypy and SPD, basic symptoms decidedly have state character, as, by definition, they differ from what patients consider to be their “normal” mental self . Basic symptoms are conceptualized as the earliest primary psychopathological correlates of the neurophysiological disturbances of information processing underlying the development of attenuated and frank psychotic symptoms, which develop based on and partly in reaction to basic symptoms . Thus, independently of any thought content or perception, basic symptoms are disturbances in mental processes themselves, thereby clearly differing from more content-related positive features of schizotypy and SPD, and attenuated and brief limited psychotic symptoms .
Studies of personality dimensions, schizotypy, PDs, and SPD, in CHR samples indicate the following:
#mentalhealth Myth Buster: Schizophrenics Have Multiple Personality Disorder
Schizophrenia is one of the oldest mental illnesses known to mental health disorders. It’s also a disorder that takes on the look of several other traits of disorders at the same time. So much so that many people think it’s part of another mood disorder or oftentimes, a personality disorder.
I can’t tell you how many times I’ve heard people loosely use “schizophrenia” as a lay term for multiple personality disorder and assume they are one in the same. And because of the misunderstanding of these persistent mental illnesses I thought it would be helpful to share some of the myths between the two and set the record straight that schizophrenia and multiple personality disorder are two distinct disorders.
Sign Up for the Black Doctor Newsletter!
1. People with schizophrenia suffer from multiple personality disorder.Absolutely not true! The two major components of schizophrenia are delusions and hallucinations. Delusions are fixed ideas or beliefs one has that are not based in reality.
MUST READ: Halle Berry Brings Black Mental Health To Big Screen In ‘Frankie & Alice’
3. People suffering with schizophrenia are more dangerous than people suffering with multiple personality disorder. Not true! Having schizophrenia does not make someone more dangerous than having multiple personality disorder or any other disease. Though the media would like people to believe this, research has proven that people with schizophrenia commit less than 2% of crimes within the general public.
How Is Dissociative Identity Disorder Diagnosed
Making the diagnosis of dissociative identity disorder takes time. It’s estimated that individuals with dissociative disorders have spent seven years in the mental health system prior to accurate diagnosis. This is common, because the list of symptoms that cause a person with a dissociative disorder to seek treatment is very similar to those of many other psychiatric diagnoses. In fact, many people who have dissociative disorders also have coexisting diagnoses of borderline or other personality disorders, , and .
The DSM-5 provides the following criteria to diagnose dissociative identity disorder:
Did Is Sometimes Misdiagnosed
Healthcare professionals sometimes misdiagnose DID as schizophrenia.
It can be incredibly difficult to get a correct diagnosis of DID. According to research from 2016, of U.S. clinicians were able to accurately diagnose DID in an individual.
The clinicians misdiagnosed the condition as:
Articles On Schizophrenia Stereotypes
There’s a lot of incorrect info out there about . Some of it is spread by movies or TV shows. Or sometimes, people use stereotypes when talking about this mental illness.
is a serious mental disorder that affects your ability to think and act clearly. When you have schizophrenia, your brain often tells you you’re seeing things or hearing voices that aren’t there. This makes it hard to tell what’s real and what isn’t. It also affects how well you think, make decisions, and manage your emotions.
Around 1% of people in the U.S. have schizophrenia. It affects men and women equally. Women tend to get schizophrenia in their 20s or 30s. Men tend to get it in their late to early 20s. It’s rare in kids younger than 12. And it usually doesn’t appear for the first time in adults over 40.
If you get schizophrenia, you might have:
- , or false beliefs that don’t change, even when you’re given new ideas and facts
- A hard time remembering things
- Disordered thoughts
- , or hearing voices, seeing things, or smelling things others can’t
- Lack of emotion in your face or voice
- Problems focusing
- Trouble understanding information and making decisions
Commonly, people with schizophrenia don’t know they have it, which can make treatment much more challenging.
Get the real story behind some common myths.
A person with schizophrenia doesn’t have two different personalities. Instead, they have false ideas or have lost touch with reality. Multiple personality disorder is unrelated.
What Is Dissociative Identity Disorder
Dissociative identity disorder is a mental health condition. People with DID have two or more separate identities. These personalities control their behavior at different times. Each identity has its own personal history, traits, likes and dislikes. DID can lead to gaps in memory and hallucinations .
Dissociative identity disorder used to be called multiple personality disorder or split personality disorder.
DID is one of several dissociative disorders. These disorders affect a person’s ability to connect with reality. Other dissociative disorders include:
- Depersonalized or derealization disorder, which causes a feeling of detachment from your actions.
- Dissociative amnesia, or problems remembering information about yourself.
Myth #3: People With Schizophrenia Have Multiple Personalities
This is another myth that refuses to die. In fact, according to a 2008 study by the National Alliance on Mental Illness, 64% of people still believe schizophrenia means having multiple personalities. While people with multiple personalities do exist, most do not live with schizophrenia. The condition people are actually thinking about is called dissociative identity disorder .
Part of the reason why people believe schizophrenia is the same as dissociative identity disorder is because schizophrenia derives from a Greek word meaning “split mind.” The “split mind” aspect refers to how people with schizophrenia have minds that tend to isolate them from the rest of the world, as if they were split off. The phrase doesn’t mean the mind itself is split.
Symptoms Of Dissociation In Ssds
Several studies examined symptoms of dissociation in schizophrenia spectrum patients through the Dissociative Experiences Scale , which is the most commonly used instrument for measuring dissociation. The questionnaire contains 28 items describing dissociative experiences. The respondent is asked to state how often they had each experience ranging from 0% to 100% of the time, resulting in mean scores ranging from 0 to 100. Mean scores for healthy controls ranged between 4.38 and 14.86, whereas mean scores of patients with a DD ranged between 24.9 for depersonalization disorder and 57.06 for multiple personality disorder .
What Are Complications Of Dissociative Identity Disorder
As with other mental health conditions, the prognosis for people with DID becomes much less optimistic if not appropriately treated. Individuals with a history of being sexually abused, including those who go on to develop dissociative identity disorder, are vulnerable to abusing alcohol or other substances as a negative way of coping with their victimization. People with DID are also at risk for attempting more than once. Violent behavior has a high level of association with dissociation as well. Other debilitating outcomes of DID, like that of other severe chronic mental illnesses, include inability to obtain and maintain employment, poor relationships with others, and therefore overall lower productivity and quality of life.
Personality Traits And Disorders And Psychosis
Psychoses and schizophrenia-spectrum PD, particularly SPD, are linked historically, phenomenologically, and through shared genetic and biological factors . This link is mirrored by SPD’s placement within the ICD section for schizophrenia and related disorders and its mentioning as a related disorder in the schizophrenia section of DSM-5 . Because SPD and schizotypy—as well as other terms often used in this context such as psychotic-like experiences —are not synonymous ; in the following, we will strictly distinguish between these terms and elucidate their conceptual differences later in the manuscript .
Table 1 Current operationalizations of schizotypy, schizotypal disorder according to ICD-10, SPD and other schizophrenia-spectrum PD according to DSM-5, clinical high risk of psychosis and psychosis .
What Youll Learn To Do: Explain Symptoms And Potential Causes Of Schizophrenic And Dissociative Disorders
Figure 1. Speaking in word salad, or random words strung together without meaning, is sometimes characteristic of schizophrenia.
Schizophrenia is a severe disorder characterized by a complete breakdown in one’s ability to function in life; it often requires hospitalization. People with schizophrenia experience hallucinations and delusions, and they have extreme difficulty regulating their emotions and behavior. Thinking is incoherent and disorganized, behavior is extremely bizarre, emotions are flat, and motivation to engage in most basic life activities is lacking.
Schizophrenia is not to be confused with multiple personality disorder, which is technically termed dissociative identity disorder. The main characteristic of dissociative disorders is that people become dissociated from their sense of self, resulting in memory and identity disturbances. Dissociative disorders listed in the DSM-5 include dissociative amnesia, depersonalization/derealization disorder, and dissociative identity disorder. A person with dissociative amnesia is unable to recall important personal information, often after a stressful or traumatic experience. In this section, you’ll learn about the differences between schizophrenia and these disorders.
Dissociative Disorders: Between Neurosis And Psychosis
C. Devillé
1Department of Mental Health and Psychiatry, General Psychiatry Department, University Hospital of Geneva, CAPPI Jonction, Rue des Bains 35, 1205 Geneva, Switzerland
Abstract
Dissociative disorders are a set of disorders defined by a disturbance affecting functions that are normally integrated with a prevalence of 2.4 percent in industrialised countries. These disorders are often poorly diagnosed or misdiagnosed because of sharing common clinical features with psychotic disorders, but requiring a very different trajectory of care. Repeated clinical situations in a crisis centre in Geneva provided us with a critical overview of current evidence of knowledge in clinical and etiopathological field about dissociative disorders. Because of their multiple expressions and the overlap with psychotic disorders, we focused on the clinical aspects using three different situations to better understand their specificity and to extend our thinking to the relevance of terms “neurosis” and “psychosis.” Finally, we hope that this work might help physicians and psychiatrists to become more aware of this complex set of disorders while making a diagnosis.
1. Introduction
According to ICD-10, there are more subtypes of diagnostic categories and depersonalization/derealization disorder is classified in neurotic disorders .
2. Clinical Vignettes
2.1. Clinical Vignette Number 1
2.2. Clinical Vignette Number 2
2.3. Clinical Vignette Number 3
3. Discussion
4. Conclusion
For Those With Did Medication Rarely Helps At All
Muller said drugs “can help a little bit,” with DID, but certainly do not help a lot.
“Many drugs have been tried, but nothing really seems to help that much drug-wise,” he said. “Some of the drugs can numb the pain a little bit, so you get some people with DID on anti depressants, like Prozac. It can take some of the edge off, but it certainly doesn’t cure the altered states of consciousness, or dissociating.”
Whatever level of DID a patient has, drugs don’t make it go away, or even change it in any way. Muller says it’s the psychotherapy which can really help people.
He said need therapists who understand trauma to help them deal with the memories of the past without getting badly triggered by them. He mentions and explains some of the concepts of trauma in his book “.”
DID is on the same spectrum as post traumatic stress disorder , and so a big part of the therapy is digging into the past to find out where the trauma was, to face it, and to learn what it is in day to day life that might bring it back and make the patient fearful.
Nothing necessarily bad has to be happening to someone with DID to trigger dissociation either. It might be the way a room is lit, a topic brought up in a book or a film, or the sight of a particular item of clothing. It’s just that something about the situation is similar to the one where they were incredibly scared, and their brain starts protecting them again.
Can Someone Have Schizophrenia Bipolar And Multiple Personality Disorder At The Same Time
Dr. Heidi Fowlerpersonality disorderDr. Andrew Ho
Ask U.S. doctors your own question and get educational, text answers — it’s anonymous and free!
Ask U.S. doctors your own question and get educational, text answers — it’s anonymous and free!
HealthTap doctors are based in the U.S., board certified, and available by text or video.
Early Warning Signs Of Schizophrenia
In some people, schizophrenia appears suddenly and without warning. But for most, it comes on slowly, with subtle warning signs and a gradual decline in functioning, long before the first severe episode. Often, friends or family members will know early on that something is wrong, without knowing exactly what.
In this early phase of schizophrenia, you may seem eccentric, unmotivated, emotionless, and reclusive to others. You may start to isolate yourself, begin neglecting your appearance, say peculiar things, and show a general indifference to life. You may abandon hobbies and activities, and your performance at work or school can deteriorate.
Schizophrenia: The 7 Keys To Self
Seek social support. Friends and family vital to helping you get the right treatment and keeping your symptoms under control. Regularly connecting with others face-to-face is also the most effective way to calm your nervous system and relieve stress. Stay involved with others by continuing your work or education. If that’s not possible, consider , joining a schizophrenia support group, or taking a class or joining a club to spend time with people who have common interests. As well as keeping you socially connected, it can help you feel good about yourself.
Manage stress. High levels of stress are believed to trigger schizophrenic episodes by increasing the body’s production of the hormone cortisol. As well as staying socially connected, there are plenty of steps you can take to reduce your stress levels. Try adopting a regular relaxation practice such as yoga, deep breathing, or .
Get regular exercise. As well as all the emotional and physical benefits, exercise may help reduce symptoms of schizophrenia, improve your focus and energy, and help you feel calmer. Aim for 30 minutes of activity on most days, or if it’s easier, three 10-minute sessions. Try rhythmic exercise that engages both your arms and legs, such as walking, running, swimming, or dancing.
How Is Did Different From Schizophrenia
There are a lot of misconceptions surrounding both and . Many people inaccurately believe that people with schizophrenia have “split personalities.” This isn’t the case.
This isn’t even technically true of DID. The Sidran Institute says that, although these personalities may feel or appear different, “They’re all manifestations of a single, whole person.”
While some symptoms do overlap between DID and schizophrenia, they are different in important ways, including their causes, treatments, and age of onset.
Schizophrenia: Early Warning Signs
Early detection and treatment of conditions such as heart disease and cancer have improved survival rates and quality of life for people who suffer from these conditions. A new approach involves identifying people who show minor symptoms of psychosis, such as unusual thought content, paranoia, odd communication, delusions, problems at school or work, and a decline in social functioning—which are coined prodromal symptoms—and following these individuals over time to determine which of them develop a psychotic disorder and which factors best predict such a disorder. A number of factors have been identified that predict a greater likelihood that prodromal individuals will develop a psychotic disorder: genetic risk , recent deterioration in functioning, high levels of unusual thought content, high levels of suspicion or paranoia, poor social functioning, and a history of substance abuse . Further research will enable a more accurate prediction of those at greatest risk for developing schizophrenia, and thus to whom early intervention efforts should be directed.
Can One Individual Be Both Did And Bipolar
What is the real meaning behind Dissociative Identity Disorder ?
Dissociative Identity Disorder, also known as DID, or sometimes referred to as Multiple Personality Disorder, is a split in an individual’s identity characterized by two or more occurring personalities in one individual. It is characterized by each personality having their own effect, age, behavior, consciousness, memory and perception of life. These characteristics are based on one’s experiences in a lifetime. In some cases there is a difference in the voice of one alter from another alter. An example would be that of a young child alter would sound more childlike and/or would use more childlike grammar than an older alter. Often the lifestyles and even speech patterns are not consistent with the real age of the individual.
Individuals with DID experience lapses or spaces in their past personal memory. For instance, one alter may go to the store, but once inside the store, another alter comes out, takes control of the body, does the shopping according to their unique likes and dislikes, and then proceeds to drive home. Once at home, the second alter, who did the shopping goes back inside, and the previous alter now comes back into control.
Causes and Experiences of DID
How can we be sure of these facts?
I can be sure, and you can be sure too, because I am a living example.
What is Bipolar Disorder?
#3 Myth: People With Schizophrenia Cant Ever Hold Down A Job
Reality: Actually, some individuals, when stable, are able to function quite well, Dr. Rego says. “When they are being compliant with their medication and are engaged in some sort of psychosocial treatment, they are often quite functional,” he says. The National Alliance on Mental Illness estimates that as many as half of the two million Americans with schizophrenia can improve significantly or even recover completely if they get treatment. Dr. Rego refers to the “recovery model” of treatment for schizophrenia, and an article in the Current Opinion in Psychiatry.
“Working appears to help people recover from schizophrenia, and recent advances in vocational rehabilitation have been shown to be effective in countries with differing economies and labor markets. A growing body of research supports the concept that empowerment is an important component of the recovery process,” the authors write.
If A Friend Or Family Member Has Did How Can I Help
Having a loved one with DID can be confusing and overwhelming. You may not know how to respond to their different alters or behaviors. You can help by:
- Learning about DID and its symptoms.
- Offering to attend family counseling or support groups with your loved one.
- Staying calm and supportive when sudden behavior changes occur.
What’s The Treatment Plan For Dissociative Identity Disorder
There are currently no formal, evidence-based guildelines to treat DID. Many treatments are based on case reports or are even controversial.
While there’s also no “cure” for dissociative identity disorder, long-term treatment can be helpful, if the patient stays committed. Effective treatment includes:
- Psychotherapy: Also called talk therapy, the therapy is designed to work through whatever triggered and triggers the DID. The goal is to help “fuse�? the separate personality traits into one consolidated personality that can control the triggers. This therapy often includes involving family members in the therapy.
- Hypnotherapy. Used in conjunction with psychotherapy, clinical hypnosis can be used to help access repressed memories, control some of the problematic behaviors which accompany DID as well as help integrate the personalities into one.
- Adjunctive therapy. Therapies such as art or movement therapy have been shown to help people connect with parts of their mind that they have shut off to cope with trauma.
There are no established treatments for dissociative identity disorder, making psychologically-based approaches the mainstay of therapy. Treatment of co-occurring disorders, such as or substance use disorders, is fundamental to overall improvement. Because the symptoms of dissociative disorders often occur with other disorders, such as anxiety and , medicines to treat those co-occurring problems, if present, are sometimes used in addition to psychotherapy.