Free Brochures And Shareable Resources
- Helping Children and Adolescents Cope With Traumatic Events: This fact sheet presents information on how children and adolescents respond to traumatic events, and what family, friends, and trusted adults can do to help. Also available en español.
- Post-Traumatic Stress Disorder: This brochure provides information about post-traumatic stress disorder including what it is, who develops PTSD, symptoms, treatment options, and how to find help for yourself or someone else who may have PTSD. Also available en español.
- : Help support PTSD awareness and education in your community. Use these digital resources, including graphics and messages, to spread the word about PTSD.
Can You Have Both
The simple answer is yes. While not everyone who experiences trauma will have PTSD, having another mental health diagnosis, including bipolar disorder, may put a person at risk of developing PTSD.
Its possible for some people with bipolar disorder to develop PTSD from a traumatizing event or events or for a person who has PTSD to receive a diagnosis of bipolar disorder.
Ptsd And Dissociative Disorders
Dissociation is a common result of trauma.
According to the American Psychiatric Association, about 90% of people with dissociative disorders have experienced childhood abuse and neglect.
Dissociation is a disconnect between your thoughts, memories, emotions, and sense of self. It can happen during a traumatic event as your bodys way of distancing yourself from a very difficult situation. Dissociation can also arise long after the traumatic event has ended.
Each persons experience of dissociation may be slightly different. Two major types of dissociation are:
- Depersonalization: where you feel disconnected from your body. Some describe it as an out-of-body experience.
- Derealization: where people or objects around you appear unreal. The world may appear unnatural.
There are three types of dissociative disorder:
Don’t Miss: Can Someone With Schizophrenia Work
Diagnostic And Statistical Manual
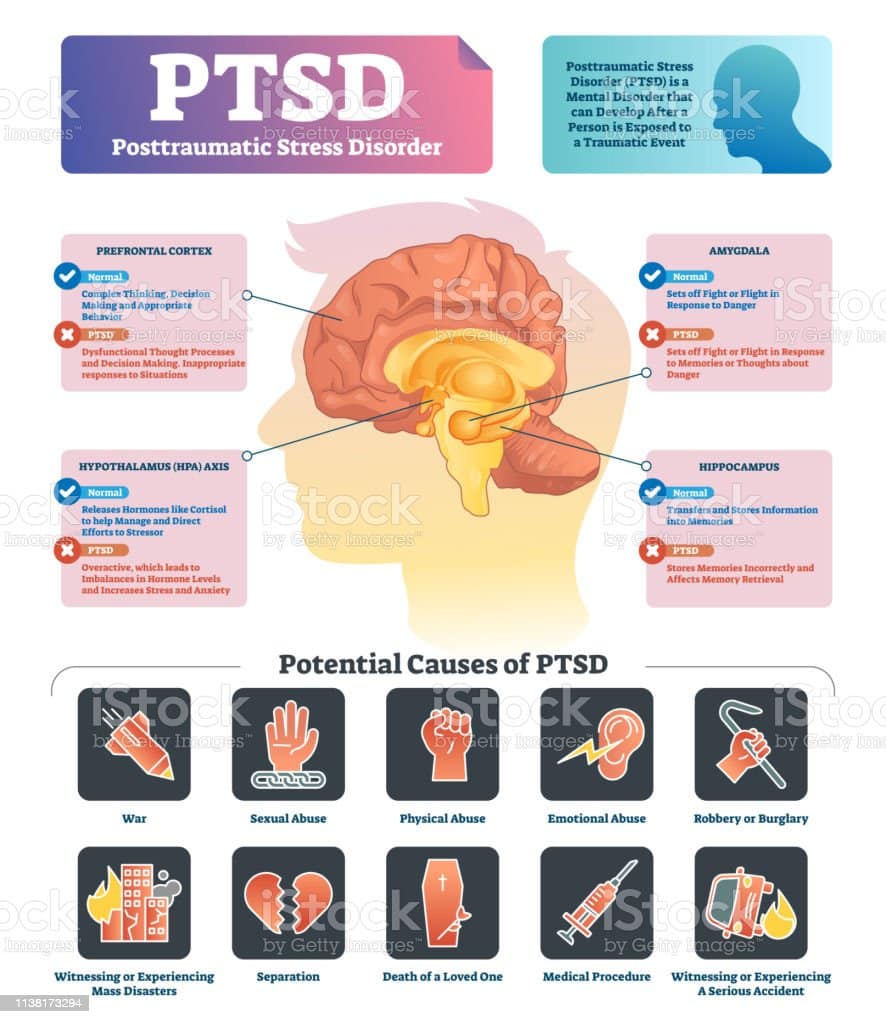
PTSD was classified as an anxiety disorder in the DSM-IV, but has since been reclassified as a “trauma- and stressor-related disorder” in the DSM-5. The DSM-5 diagnostic criteria for PTSD include four symptom clusters: re-experiencing, avoidance, negative alterations in cognition/mood, and alterations in arousal and reactivity.
What Is A Mental Illness
According to The American Heritage® Stedman’s Medical Dictionary, mental illness” is defined as:
Any of various disorders characterized chiefly by abnormal behavior or an inability to function socially, including diseases of the mind and personality and certain diseases of the brain. Also called mental disease, mental disorder.
In the case of those who have PTSD, they experience significant, abnormal behavior. Examples of this might be diving to the floor when a car backfires or feeling as though they are reliving the traumatic events, even to the point of hallucinating .
Read Also: What To Do To Calm Down From A Panic Attack
How Does Therapy Help
Trauma therapy gives kids a way to safely share their feelings, tell their story, and get support.
In therapy, kids learn coping and calming skills to help them deal with anxiety they feel after a trauma. This makes it easier to talk about what theyve been through.
Through therapy, kids learn to adjust some of their thoughts about the trauma. They learn to let go of any guilt or shame about what happened to them. Slowly, they learn to face things they used to avoid.
Therapy helps children gain courage and confidence. Kids use their strengths to cope.
How Can I Help My Child Live With Ptsd
As a parent, you play a key role in your childs treatment. Here are things you can do to help:
-
Admit that the event happened. Pretending everything is normal won’t help your child.
-
Be supportive and get counseling for children and teens who have seen or gone through a traumatic event. A child or teen may at first not want counseling. But it may be needed months or even years after the traumatic event.
-
Keep all appointments with your child’s healthcare provider.
-
Talk with your childs healthcare provider about other providers who will be included in your childs care. Your child may get care from a team that may include counselors, therapists, social workers, psychologists, and psychiatrists. Your childs care team will depend on his or her needs and how serious the PTSD is.
-
Tell others about your childs PTSD. Work with your childs healthcare provider and school to create a treatment plan.
-
Reach out for support from local community services. Being in touch with other parents who have a child with PTSD may be helpful.
-
Take all symptoms of depression and suicide very seriously. Get treatment right away. Suicide is a health emergency.
Recommended Reading: Can You Have Mild Schizophrenia
Is There A Difference Between Ptsd And Ptss
When comparing PTSS vs. PTSD, the main difference is that PTSS is not a legitimate mental health disorder like PTSD. Rather, it is a precursor to PTSD. PTSS is a reaction or symptoms that occur earlier than 30 days after experiencing a traumatic event.
As a result, PTSS is now being recognized as a serious health concern. Even so, PTSS often goes unrecognized until a PTSD diagnosis is made.
Screening tools like the PTSS-14 are reliable in identifying people with PTSS who are at a high risk of developing PTSD. Through earlier recognition, providers may be able to intervene and alleviate or reduce the effects of the traumatic experience and the likelihood of a PTSD diagnosis.
Why Are Traumatic Events So Shocking
Traumatic events are shocking because we cannot make sense of them. They dont fit with our sense of what the world should be like.
Traumatic events often appear to be random or dont have a clear cause. They do not fit in with our views about how the world should be, which can make it difficult for us to understand the meaning behind them.
Traumatic experiences also show us that bad things can happen to us and the people we care about at any time. This can lead to us feeling unsafe and threatened which is understandably frightening. Sometimes traumatic events can make us question who we are, which can be distressing too.
Read Also: What Part Of Brain Does Schizophrenia Affect
When Should I Call My Childs Healthcare Provider
-
Feels extreme depression, fear, anxiety, or anger toward him or herself or others
-
Feels out of control
-
Hears voices that others dont hear
-
Sees things that others dont see
-
Cant sleep or eat for 3 days in a row
-
Shows behavior that concerns friends, family, or teachers, and others express concern about this behavior and ask you to get help
PTSD increases risk for other mental health disorders, including depression, anxiety, and suicidal thinking.
Posttraumatic Stress Disorder In The Dsm
Between the DSM-IV and the DSM-5, there have been some changes to the criteria for PTSD. Currently, there are considered to be eight criteria for a PTSD diagnosis. The first of the PTSD criteria include:
- Directly experiencing the traumatic event
- Witnessing, in person, the event as it occurred to others
- Learning that the traumatic event occurred to a close family member or friend
- Experiencing repeated or extreme exposure to aversive details of the traumatic event this does not apply to exposure through media such as television, movies, or pictures
The second PTSD criterion consists of symptoms involving re-experiencing:
- Thoughts or perception
- Dissociative flashback episodes
- Intense psychological distress or reactivity to cues that symbolize some aspect of the event
The third criterion for a PTSD diagnosis involves the avoidance of stimuli that remind the person of the traumatic event:
- Avoidance of thoughts, feelings, or conversations associated with the event
- Avoidance of people, places, or activities that may trigger recollections of the event
The fourth of the PTSD criteria involves persistent negative thoughts, mostly associated with the traumatic event:
The fifth of the PTSD diagnosis criteria involves an increase in arousal and reactivity:
- Irritable behavior and angry outbursts
- Reckless or self-destructive behavior
Also Check: What Its Like To Have An Eating Disorder
Ptsd In Military Veterans
For all too many veterans, returning from military service means coping with symptoms of PTSD. You may have a hard time readjusting to life out of the military. Or you may constantly feel on edge, emotionally numb and disconnected, or close to panicking or exploding. But its important to know that youre not alone and there are plenty of ways you can deal with nightmares and flashbacks, cope with feelings of depression, anxiety or guilt, and regain your sense of control.
When Is It Diagnosed
When you go through something you find traumatic it’s understandable to experience some symptoms of PTSD afterwards, such as feeling numb or having trouble sleeping. This is sometimes described as an ‘acute stress reaction’.
Many people find that these symptoms disappear within a few weeks, but if your symptoms last for longer than a month, you might be given a diagnosis of PTSD. Your GP might refer you to a specialist before this if your symptoms are particularly severe.
I started experiencing symptoms of PTSD after my boyfriend died. I suffered extremely vivid flashbacks that could happen at any time, anywhere, and were deeply distressing I threw myself into another relationship very quickly to try and avoid how I was feeling, but then also would not express much affection to my new partner.
Also Check: What To Say When Calling In Sick With Anxiety
What Happens When Someone Has Ptsd
Many people will experience traumatic events throughout their lives. About one third of adults in England report having experienced at least one traumatic event. However, not everyone who experiences a traumatic event will go on to develop PTSD.
Many people can experience grief, sadness, anxiety, guilt and anger after a traumatic experience. This does not necessarily mean that someone has PTSD. People who have PTSD often have many of the following symptoms. These can start immediately, or they might take some weeks or even months to begin.
With PTSD, these symptoms will interfere with your day-to-day activities and/or cause you to feel extremely distressed. If you have any of these symptoms immediately after a traumatic event, this does not necessarily mean that you will develop PTSD.
Why Doesn’t Everyone Get Ptsd After A Traumatic Experience
After a traumatic experience, many people will have some trauma symptoms for the first month or so. Many of these symptoms are normal reactions to experiencing real or perceived danger. You can think about them as your brains way of protecting you from harm.
However, most people will process what has happened after a few weeks, or sometimes a little longer, and their stress symptoms will start to disappear.
Research shows that certain groups of people are at increased risk of developing PTSD. The risk of developing PTSD is decreased if someone can:
- access social support and
- causes mutilation
- involves children.
If you continue to be exposed to stress and uncertainty, this will make it more difficult for your PTSD symptoms to improve.
You may have got over a traumatic event if you can:
- think about it without becoming overly distressed
- not feel constantly under threat
- not think about it at inappropriate times.
There are a number of reasons why someone with PTSD might not be diagnosed.
You May Like: How To Cope With Depression During Pregnancy
What Are The Symptoms Of Post
There are four types of PTSD symptoms, but they may not be the same for everyone. Each person experiences symptoms in their own way. The types are:
- Re-experiencing symptoms, where something reminds you of the trauma and you feel that fear again. Examples include
- Flashbacks, which cause you to feel like you are going through the event again
- Frightening thoughts
The symptoms usually start soon after the traumatic event. But sometimes they may not appear until months or years later. They also may come and go over many years.
When Does Ptsd Start
The symptoms of PTSD can start immediately after a traumatic event, or even weeks or months afterwards. Usually, symptoms start within 6 months of the event. Sometimes symptoms will start after 6 months, though this is less common. Unfortunately, many people will not ask for help when their symptoms first start.
PTSD cannot be diagnosed in the first month after a traumatic event. If you experience trauma symptoms straight away, and these are severe and prevent you from functioning, you might be experiencing an ‘acute stress disorder’.
Recommended Reading: How To Treat Dog Panic Attacks
Support Is Important For Recovery
Many people experience some of the symptoms of PTSD in the first two weeks after a traumatic event, but most recover with the help of family and friends. For this reason, for a diagnosis of PTSD is not made until a month after the event. Treatment does not usually start for at least two or more weeks after a traumatic experience. However if the event is very distressing and emotions and reactions are intense, it is advisable to seek help as early as possible to understand what is happening and help recovery to start.
It is important during the first few days and weeks after a traumatic event to get whatever help is needed. This may include accessing information, people and resources that can help you to recover. Support from family and friends may be all that is needed. Otherwise, a doctor is the best place to start to get further help.
How Ptsd Is Treated
PTSD can be successfully treated, even when it develops many years after a traumatic event.
Any treatment depends on the severity of symptoms and how soon they occur after the traumatic event. Any of the following treatment options may be recommended:
- Watchful waiting monitoring your symptoms to see whether they improve or get worse without treatment.
- Psychotherapy such as trauma-focused cognitive behavioural therapy or eye movement desensitisation and reprocessing .
- Antidepressants such as paroxetine or mirtazapine.
Read more about treating PTSD.
You May Like: What Pills Do You Take For Bipolar
Impact Of Ptsd On Relationships And Day
PTSD can affect a personâs ability to work, perform day-to-day activities or relate to their family and friends. A person with PTSD can often seem uninterested or distant as they try not to think or feel in order to block out painful memories. They may stop them from participating in family life or ignore offers of help. This can lead to loved ones feeling shut out.
It is important to remember that these behaviours are part of the problem. People with PTSD need the support of family and friends but may not understand what is happening to them or think that they need help.
When PTSD goes on for some time, it is not unusual for people to experience other mental health problems at the same time. In fact, up to 80 per cent of people who have long-standing PTSD develop additional problems – most commonly depression, anxiety, and alcohol or other substance misuse. These may have developed directly in response to the traumatic event or as a result of the effects of having PTSD.
How Is Anxiety Different Than Ptsd
When the average person hears anxiety, we start thinking pre-existing issues like Generalized Anxiety Disorder among others. Unlike PTSD, traumatic events dont necessarily have to happen for a person to experience anxiety symptoms. The difference between PTSD and anxiety can be tricky to pinpoint, especially when soldiers with history of mental health issues like anxiety are then exposed to extremely traumatic experiences in their military service. Their symptoms may be re-aggravated or made worse. Because every person is different and reacts differently to situations based on their coping skills, morals, values, and experiences in life reactions to those events will be different as well. Where one person may not have any lasting mental health condition to an event, another may develop PTSD. We do not know what causes one person to develop certain conditions and others to not, but we continue to try to understand and treat them.
Recommended Reading: How To Deal With A Depressive Episode
Can You Be Diagnosed With Ptsd And Anxiety Together
While yes that is a possibility since a veteran with a history of anxiety before service could have been exposed to a traumatic experience in active duty, we still have to consider several factors. A common issue with differentiating between mental health conditions is that many of them have very similar symptoms . That makes it so challenging to determine, especially in one session, which diagnosis a veteran may have. Add the fact that most of us do not want to go into a room and talk to a stranger about our most traumatic life events, and then the diagnosis can get even more challenging to make. This is why we see veterans diagnosed with one condition, then later be diagnosed with a different one, or an additional one, or two. There are also theories that some chronic trauma disorders such as PTSD cause a person to create coping skills that mimic other disorders such as Borderline Personality disorder or Bipolar disorder. If someone has been coping with PTSD for several years, or even decades, often times they have created coping mechanisms that hide their symptoms so well they are misdiagnosed with other disorders they may not actually have originally had but developed as a protective measure.