Risks And Complications Of Schizophrenia
Though the cause of schizophrenia is still unknown, researchers have found certain factors that have proven to increase the risk of schizophrenia in patients. These risk factors include the following conditions:
- Birth complications at the fetal stage or during delivery
- Infection of the central nervous system during infancy or early childhood
- Childhood trauma like having to witness the death of a family member
- Social stresses like economic troubles or family separations
Even though these risk factors can increase the chances of an individual being diagnosed with schizophrenia, many patients are often seen who have not been exposed to these aspects of their life.
Schizophrenic disorders are a severe mental illness that can lead to several complications throughout life. The mental disorder needs lifelong treatment and should not be left untreated. The most common complications that might arise are:
- Attempts of self-injury and suicide
- Development of phobias
- Social anxiety in day-to-day tasks
- Depression and feelings of hopelessness
- Troubles with personal relationships and family
Schizophrenia makes it difficult for people to attend school or work, giving rise to financial problems too.
Full Recovery From Schizophrenia
This is the first of a series of blog postings related to my own series of research studies of people who have made full and lasting medication-free recoveries after being diagnosed with schizophrenia and other psychotic disorders. This is very exciting research because it is one of the few areas within psychological research that remains almost completely wide open. One reason it is so wide open is that most Westerners donât believe that genuine recovery from schizophrenia and other related psychotic disorders is possible, in spite of significant evidence to the contrary. Since there are some very hopeful findings that have emerged within this research, I want to begin this series of postings by summing up one particularly hopeful aspect of my own research, which is a group of five factors that emerged which are considered to have been the most important factors in my participantsâ recovery process. But before looking closer at these factors, we should back up for a minute
This takes us to Factor #2: Arriving at an understanding of their psychosis alternative to the brain disease theory. Every participant went through a process of developing a more hopeful understanding of their psychotic experiences, generally coming to see their psychosis as a natural though very risky and haphazard process initiated by their psyche in an attempt to cope and/or heal from a way of being in the world that was simply no longer sustainable for them.
References
Research On Psychotherapy Of Schizophrenia
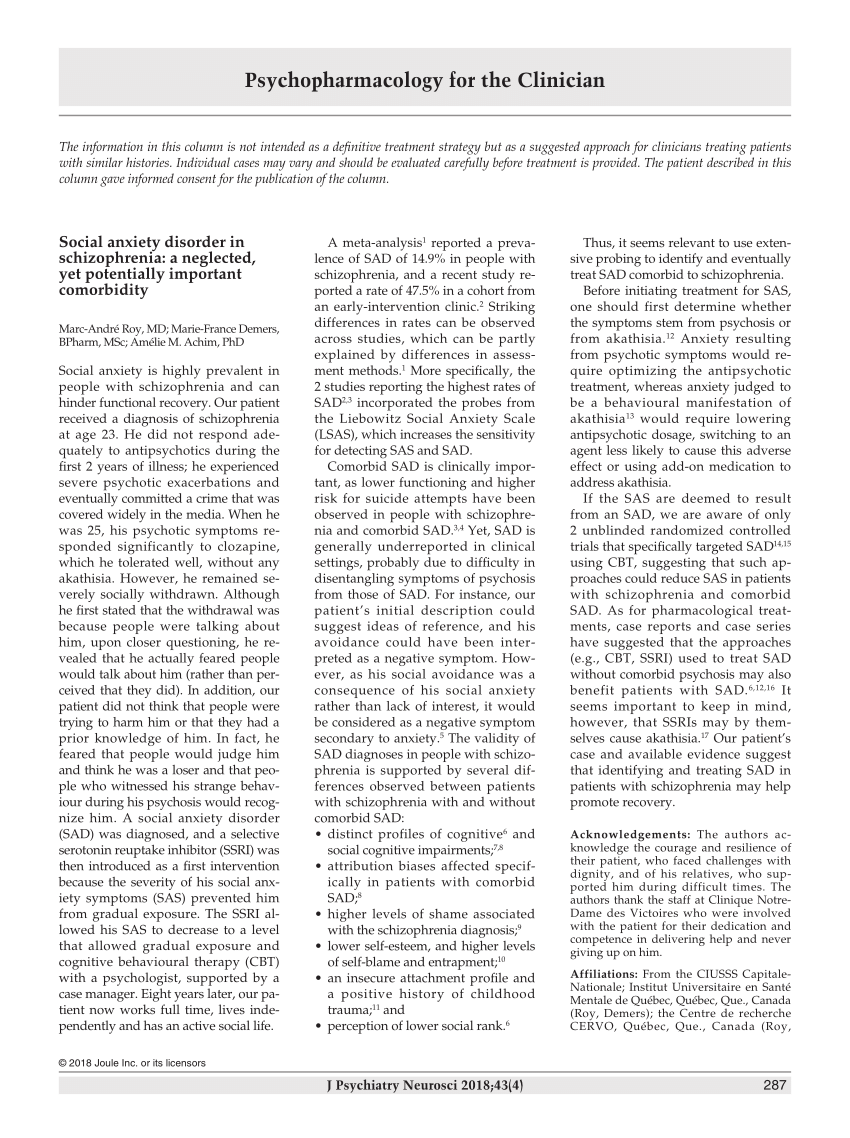
One of the first clinicians to advocate for individual psychotherapy for people with schizophrenia was Carl , who treated many hospitalized patients at the Burghölzli Hospital in the early part of the 20th century. Jung noted that many people with schizophrenia are amenable to therapy, but that caution must be used because under certain conditions, therapy could cause an increase in symptoms . In an analysis of an early case, Jung described how the patient describes for us, in her symptoms, the hopes and disappointments of her life . This statement demonstrates Jungs view that symptoms, even bizarre ones, are linked to the life history and self-concept of the patient, and that much of the work of therapy involves increasing psychological understanding and redefining the self-concept. Once Jung left the Burghölzli, however, he rarely treated people with schizophrenia, and with a few notable exceptions , this was true of his followers as well. Moreover, with the growth of psychoanalysis, and claim that persons with schizophrenia could not benefit from psychoanalysis due an inability on their part to form deep attachments with others, psychotherapy for schizophrenia was virtually nonexistent by the middle of the 20th century.
Perhaps even more compelling than these data and suggestions, however, is that recent theoretical developments suggest new methods and mechanisms by which psychotherapy for schizophrenia might be effective. These are discussed in the section below.
You May Like: Schizophrenia Cycles
Future Research: Three Related Foci
Turning to the issue of metacognition, we would envision a psychotherapy that might promote recovery by providing a place in which clients may develop their capacities to think about thinking. This might well involve offering opportunities to practice acts of metacognition leading to the strengthening of the ability to perform metacognitive acts of increasing complexity. As discussed by , psychotherapy can provide many opportunities for this, in terms of examining and monitoring: 1) attributions regarding self and others 2) symptoms and mental states 3) schemata-linked habitual reaction patterns in thinking and behavior and 4) thoughts and feelings about all parts of the self. And, as suggested by psychotherapy is thus one method in which different kinds of metacognition capacity are regularly assessed and intervention is accordingly staged to match clients capacities.
The development and definition of such treatments would seem likely to be able to draw from a range of existing procedures and by definition be integrative in nature. For instance, cognitive behavior therapy for psychosis has been used to address the personal meaning of symptoms as well as awareness of the process of thinking beyond the correction of maladaptive beliefs . The incorporation of methodologies which target metacognition in other groups could also enrich and speed the process of definition and testing of such an intervention.
Coping And Support Techniques We Use
Psychosocial Rehab Aimed at reintegrating patients back into society to find purpose and dignity.
Developing awareness and understanding Awareness about various aspects, such as causes and treatment of schizophrenia
Specific treatment goals Milestone based treatment plans to keep patients motivated
Support help groups Sharing individual experiences with a group of similar people
Stress management and relaxation techniques Relaxation techniques such as yoga and meditation may help
Read Also: What’s The Phobia Of Throwing Up
How Doctors Diagnose It
There are no lab tests to find schizophrenia, so doctors usually base a diagnosis on a personâs history and symptoms. They will first rule out other medical causes. In teens, a combination of family history and certain behaviors can help predict the start of schizophrenia. The period when symptoms first start to arise and before the first episode of psychosis is called the prodromal period. It can last days, weeks or even a years. Sometime it can be difficult to recognize because there is usually no specific trigger. Prodrome is accompanied by what can be perceived as subtle behavioral changes, especially in teens. These behaviors include withdrawing from social groups and expressing unusual suspicions, but thatâs not enough for a diagnosis.
John Nash’s Genius Is Extraordinary Recovering From Schizophrenia Is Anything But
The end of “A Beautiful Mind,” the Oscar-nominated movie based loosely on the life of Nobel Prize winner John Forbes Nash Jr., depicts the Princeton mathematician’s emergence from the stranglehold of paranoid schizophrenia, the most feared and disabling of mental illnesses. Moviegoers who have watched the cinematic metamorphosis of actor Russell Crowe from the disheveled genius who furiously covers his office walls with delusional scribblings to the silver-haired academic perfectly at home in the rarefied company of fellow laureates in Stockholm might assume that Nash’s recovery from three decades of psychosis is unique.
But mental health experts say that while Nash’s life is undeniably remarkable, his gradual recovery from schizophrenia is not.
That contention is likely to surprise many people, including some psychiatrists, who continue to believe the theory, promulgated a century ago by Sigmund Freud and his contemporaries, that the serious thought and mood disorder is a relentless, degenerative illness that robs victims of social and intellectual function, invariably dooming them to a miserable life in a homeless shelter, a prison cell or, at best, a group home.
Recommended Reading: Clown Phobia Definition
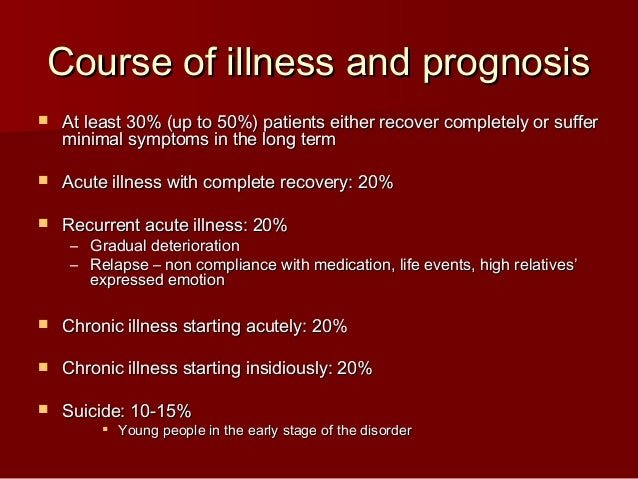
Recovery Rate Of Schizophrenia
Hi, guys!
Im looking for scientific data for a presentation and I want to know the recovery rate of schizophrenia.
I found these facts, but theyre from a book called Surviving Schizophrenia: A Manual for Family, Patients, and Providers :
After 10 years, of the people diagnosed with schizophrenia:
- 25% Completely Recover
- 25% Much Improved, relatively independent
- 25% Improved, but require extensive support network
- 15% Hospitalized, unimproved
After 30 years, of the people diagnosed with schizophrenia:
- 25% Completely Recover
- 35% Much Improved, relatively independent
- 15% Improved, but require extensive support network
- 10% Hospitalized, unimproved
- 15% Dead
Im looking for the scientific data of these stastistics. Does someone who has the book know from which scientific article they took these numbers?
Thank you in advance!
Abstract. Objective: Our primary aims were to identify the proportion of individuals with schizophrenia and related psychoses who met recovery criteria bas
Im just reading this article.
Thank you. I hope it helps.
Keep in mind when reading about this that it varies by how recovery is defined, by how populations are sampled, and by which populations are studied .
Keep in mind when reading about this that it varies by how recovery is defined,
I think that half or more of the problem. Theres no clear consensus on the issue. Even here wed probably disagree over what constitutes recovery.
Its true that there are no clear metrics to define recovery:
Toward A Concept Of Remission
A development from over 20 years ago offers a useful point of departure for our efforts to identify and understand some of the elements of this confusing picture. It was at that time that a pair of statisticians, Cohen and Cohen, first introduced the notion of the clinician’s illusion to account for the tendency among practitioners, who treat ambiguous and prolonged illnesses, to assume that the ways in which such illnesses present in clinical care settings represent the ways these illnesses look both over time and among the broader population of persons afflicted with them. Based on a combination of advanced statistics and common sense knowledge that people who are neither acutely nor severely ill are less likely to access clinical care, the Cohens’ theory offered an explanation for how and why mental health professionals might retain their traditionally narrow and negative view of outcome in a condition like schizophrenia despite the accumulation of longitudinal data which suggests otherwise. Simply stated, when people are managing their condition adequately on their own they are much less likely to seek care.
According to the members of the Remission Working Group, such a remission can be characterized as:
You May Like: Phobiadefinition
Brain Functional Abnormalities In Treatment
Functional neuroimaging techniques offer indirect ways of investigating brain activity in vivo. Functional neuroimaging data showed that a lower striatal metabolism before antipsychotics treatment was a predictor of a good clinical response and that responders patients showed a greater increase in striatal metabolism after antipsychotics therapy . A recent extensive review pointed out a pattern of hypometabolism in the PFC and hypermetabolism in the basal ganglia. Similar results support these findings for example another recent systematic review showed decreased metabolism in frontotemporal regions and increased perfusion in the basal ganglia in TRS. Moreover, some research groups investigated whether disruptions in resting-state functional connectivity were associated with TRS . Recently, in a fMRI study, Ganella et al. assessed functional brain networks abnormalities in TRS patients in comparison with healthy subjects, showing a global brain functional connectivity reduction in patients. In particular, this study revealed a decrease in temporal, occipital, and frontal region . Other studies focusing con brain connectivity performed with different paradigms lead to similar conclusion of a general functional connectivity decrease .
Schizophrenia Diagnosis And Treatment
There is no single health exam or a brain scan that can suffice for the diagnosis of schizophrenia. Since the doctors are still unaware of the exact cause of schizophrenia, to determine how to treat schizophrenia, multiple psychometric tests and exams need to be done before confirming the diagnosis. These health exams comprise of the following:
- During the initial appointment checkup, the doctor needs to know the entire medical history of the patient and their family, followed by their normal mental health, mood patterns, and substance abuse problems. They may also ask for school or work performance reports to get insights into the cognitive abilities of the patient.
- For the next step, the doctor may prescribe several blood tests, physical exam and imaging tests like Computed Tomography scan and Magnetic Resonance Imaging .
- Even psychometric assessments are essential to establish the diagnosis.
- For the final step and confirmed diagnosis, the patient should have experienced symptoms of positive schizophrenia in a one-month period. These symptoms are hallucinations, delusions, and disorganized speech.
The symptoms of schizophrenia often overlap with other mental health conditions like bipolar disorder or schizoaffective disorder. Again, other medical conditions that can also show the same type of symptoms. This is why doctors need to perform an exhaustive number of tests to rule out other issues. Some of the health disorders that have similar symptoms to schizophrenia are:
Read Also: Irrational Fear Of Bees
Brain Structural Abnormalities In Treatment
Ventricular enlargement is one of the variables most studied in TRS. Early CT studies showed an inverse relationship between degree of ventricular enlargement and antipsychotics treatment response . These findings were confirmed by subsequent CT studies, using also morphometric techniques, such as ventricular brain ratio . Over the last three decades, CT and then MRI cross sectional studies including chronic patients have found an association between ventricular enlargement and poor outcome . In particular, studies in patients whose illness is progressive and resistant to treatment have shown abnormalities such as ventricular enlargement and decrease in GM . Many subsequent studies tried to replicate these findings, but a first meta-analysis of these early studies as well as a critical review of this subject found no relationship between ventricular enlargement and treatment response in schizophrenia patients . Several longitudinal studies conducted on chronic patients or first psychotic episode patients confirmed these structural changes in the brain and found that they were progressive over the course of illness. In particular, in the first study just mentioned, it has been shown that Kraepelinian patients manifested left-sided ventricular enlargement compared to treatment responsive patients followed over the same 5-year follow-up period .
Medicines That Treat It
Prescription drugs can reduce symptoms such as abnormal thinking, hallucinations, and delusions. Some people have troubling side effects, including tremors and gaining weight. Drugs may also interfere with other medicines or supplements. But in most cases, medication is a must to treat schizophrenia.
Don’t Miss: Bipolar And Eating Disorders
Which Is Not Related To A Fuller Recovery From Schizophrenia
Factor #1: Hope in the possibility of real recovery. …
Factor #3: Finding meaning. …
Factor #4: Connecting with their aliveness. …
Factor #5: Dealing with their relationships.
This site is using cookies under cookie policy .You can specify conditions of storing and accessing cookies in your browser
Can You Recover From Schizophrenia
Is schizophrenia a life sentence or was Krapelin wrong?
When Emil Krapelin first described schizophrenia in 1898 he called it dementia praecox or premature dementia because he thought that it involved a progressive deterioration of the patients functioning over time. This view persisted for many years into the 20th century.
Dr Emil Kraepelin who first described schizophrenia in 1896.
We now know that this is not the case and that the receipt of a diagnosis of schizophrenia is not a life sentence to an existence of low achievement. 1 Many people who have suffered an episode of schizophrenia or even multiple episodes go on to recover a very high level of functioning and often to be able to re-join mainstream society.2
Rule of thirds and rule of quarters
For much of the 20th century psychiatrists thought of recovery rates from schizophrenia in terms of what was known as the rule of thirds. According to this rule of thumb about one third of those diagnosed with schizophrenia would recovery completely, a further third would be improved over time, leaving the remaining third who would not show any improvement.
With improvements in treatment methods and newer medications, this model was seen to be unrepresentative and doctors now tend to use another rule of thumb which they call the rule of quarters and which suggests the outcomes after 10 years from diagnosis.
Disparity between clinical and social outcomes in schizophrenia
Factors affecting the outcome in schizophrenia
Recommended Reading: What Is The Name Of The Phobia Of Long Words
Myths And Facts About Schizophrenia
There are many misconceptions about schizophrenia leading to questions like are schizophrenics dangerous? and can schizophrenia cause violence? Several myths about schizophrenia give rise to schizophrenia stereotypes that make it tough for the patients to cope with the already difficult disease.
Busting such myths, here are some interesting facts about schizophrenia.
Myth Schizophrenia patients seem to have multiple personalities
Fact One of the most common myths about schizophrenia is about schizophrenia causing multiple personalities. Most people believe that patients suffering from schizophrenia might have split personalities, meaning they act as two separate people. Schizophrenia multiple personalities is a myth as the patient does not have two personalities but they have lost touch with reality or have false ideas about the same. There is a condition known as Multiple Personality Disorder but it is totally unrelated to schizophrenia.
Myth Schizophrenics are dangerous
Myth If the parents have schizophrenia then the child would definitely inherit the disease
Fact Most often, the question doctors get asked is schizophrenia hereditary? As per experts, genetic factors do play a role in causing schizophrenia but if only one parent has schizophrenia, then the chances of the child getting the disease are only 10%. Notably, if more than one relative of the patient in question has schizophrenia then the risk of inheriting the disease increases.
Rehab For Schizophrenia: What Happens At Rehab
Schizophrenia recovery is possible with treatment that can help manage symptoms, live and work independently, and build satisfying relationships. Apart from medication, psychosocial treatment is also very important. For such treatment to work well, the trust factor between a patient and the mental health care profession is crucial as the patient needs to be hopeful about the recovery. Inpatient rehab facilities are apt for such treatments, as it is a stable and relaxing environment where all the medication and possible therapies are provided under one roof. It helps the mental health professional or the doctor to constantly monitor the patients condition.
At Cadabams world-class rehab facility, professionals curate a comprehensive and innovative residential treatment program designed to address Schizophrenia. Each treatment program is personalized as per the individual needs and expectations. This encourages the patients to have a contributing engagement in their recovery process.
Cadabams broad-spectrum assessments and evaluation processes are what makes it one of the finest and best schizophrenia treatment centres in India. Our clinicians use this information to design comprehensive and thoughtful treatment plans for the best possible outcome. Each plan offers individual psychotherapy and therapy groups in order to understand and heal the patients psychological and physical state.
Recommended Reading: Define Aphobia