Bipolar Disorder Due To Another Medical Or Substance Abuse Disorder
Some bipolar disorders dont have a specific pattern or dont match the three categories of disorders listed above and yet, they still align with the criteria for abnormal mood changes. For example, a person may experience mild depressive or hypomanic symptoms that last less than the specified amount for cyclothymia. Additionally, a person might experience depressive episodes, but have symptoms of mood elevation that are too mild or brief to be diagnosed as mania or hypomania.
These instances can be determined to be characteristic of bipolar disorder, but arent classified under the aforementioned types of bipolar disorder.
Who Is At Risk For Bipolar I Disorder
Virtually anyone can develop bipolar I disorder. About 2.5% of the U.S. population suffers from bipolar disorder — almost 6 million people.
Most people are in their teens or early 20s when symptoms of bipolar disorder first appear. Nearly everyone with bipolar I disorder develops it before age 50. People with an immediate family member who has bipolar are at higher risk.
Both Types Should Be Properly Treated
Since hypomania is less severe than the mania that occurs in bipolar I disorder, bipolar II is often described as “milder” than bipolar Ibut this is not completely accurate. Certainly, people with bipolar I can have more serious symptoms during mania, but hypomania is still a serious condition that can have life-changing consequences and so should be properly addressed.
In addition, research suggests that bipolar II disorder is dominated by longer and more severe episodes of depression. In fact, over time, people with bipolar II become less likely to return to fully normal functioning between episodes.
One study specifically concluded that bipolar type II was linked to a poorer health-related quality of life compared to type I. This remained true even during long periods of euthymia.
Thus, experts tend to believe that bipolar II disorder is equally disabling than bipolar I disorder because it can lead to more lifetime days spent depressed and not doing as well overall between episodes. Proper treatment should be pursued for all types of bipolar disorders, and you should work closely with your healthcare team to figure out the best treatment for you.
Also Check: Can You Faint From Anxiety
What Is The Treatment For Mania Hypomania And Depression
You can check what treatment and care is recommended for bipolar disorders on the National Institute for Health and Care Excellence website.
NICE produce guidelines for how health professionals should treat certain conditions. You can download these from their website at:
The NHS doesnt have to follow these recommendations. But they should have a good reason for not following them.
What medications are recommended?
Mood stabilisers are usually used to manage mania, hypomania and depressive symptoms.
The mood stabilisers we talk about in this factsheet are:
- Lithium
- Certain benzodiazepine medication
Mania and hypomaniaYou should be offered a mood stabiliser to help manage your mania or hypomania. Your doctor may refer to your medication as antimanic medication.
If you are taking antidepressants your doctor may advise you to withdraw from taking them.
You will usually be offered an antipsychotic first. The common antipsychotics used for the treatment of bipolar disorder are:
- Haloperidol
- Quetiapine
- Risperidone
If the first antipsychotic you are given doesnt work, then you should be offered a different antipsychotic medication from the list above.
If a different antipsychotic doesnt work, then you may be offered lithium to take alongside it. If the lithium doesnt work you may be offered sodium valproate to take with an antipsychotic. Sodium valproate is an anticonvulsive medication.
Sodium Valproate shouldnt be given to girls or young women who might want to get pregnant.
Bipolar 1 Maintenance Treatment
Following remission of an acute episode, patients may remain at high risk for relapse for up to 6 months. This period of time is considered to be part of the maintenance phase.1 Maintenance treatment for bipolar 1 should be focused on preventing the relapse of manic or depressive episodes, reducing residual symptoms, reducing suicide risk, and improving the overall quality of life for the patient. Per the American Psychiatric Association guidelines, lithium, valproate, and lamotrigine exhibit significant utility in the maintenance of bipolar disorder.2,3
Of note, for patients treated with an antipsychotic medication during a preceding acute episode, the need for ongoing antipsychotic medication should be reassessed. Antipsychotics should be discontinued upon entering maintenance therapy unless they are required for control of persistent psychosis.2,3
As a clinical resource, the American Psychiatric Association has published a quick reference guide on treating bipolar disorders.
Read Also: Side Effects Of Pristique
Medications For Rapid Cycling In Bipolar Disorder
Patients with bipolar 1 disorder may also experience rapid cycling. The DSM-5 defines rapid cycling as the presence of at least 4 mood episodes in the previous 12 months that meet the criteria for manic, hypomanic, or major depressive episodes.
Initial management of rapid cycling should involve evaluating the patient for underlying medical conditions which may contribute to cycling, such as hypothyroidism or a substance-induced disorder. Medications, particularly antidepressants, may also contribute to cycling and should be discontinued if possible.
Data suggests that lithium, valproate, or lamotrigine may be used as first-line agents to treat rapid cycling.6 If monotherapy fails, then a combination of mood stabilizers or mood stabilizers in combination with antipsychotics may be considered. Of note, rapid cycling appears to present more often in women.
Whats It Like To Have Bipolar 1
Bipolar 1 disorder significantly impacts all areas of someones life because of the intensity of moods and behaviors that accompany this illness. Manic episodes impair regular functioning in most cases, making it challenging to complete daily tasks. Work, school, family, social, and personal life are all impacted by symptoms of bipolar 1.
Everyones experience with bipolar 1 will be different, but some find that mania can feel quite good, whereas the depression almost universally feels awful. This tug-of-war between emotional highs and lows can make life almost unbearably difficult. Fluctuations in energy, focus, motivation, and thoughts make stability in daily life almost impossible when bipolar disorder is left untreated.
Manic episodes are usually noticeable to others because of the severe personality changes and impulsive behaviors associated with it. Bipolar 1 can negatively impact relationships because it can be confusing and unpredictable for someone on the outside to understand or help.
Also Check: Childhood Trauma And Bipolar Disorder
Medications For Manic Hypomanic Or Mixed Episodes
Per the American Psychiatric Associations practice guidelines,2 in cases of severe mania or mixed episodes , the initiation of either lithium plus an antipsychotic or valproate plus an antipsychotic is recommended as first line. For less ill patients, monotherapy with lithium, valproate, or an antipsychotic may be utilized. Use of depot antipsychotics may be used if the patient is not willing to take oral medications.
Several large multicentric double-blind, placebo-controlled and comparative randomized studies have supported the use of antipsychotics, including the following, in the management of acute mania:3
- olanzapine
- paliperidone
- ziprasidone
For patients with breakthrough episodes of mania or hypomania , the first step in management involves optimization of the ongoing agent. Optimization may be achieved by monitoring serum levels of agents such as lithium or valproate. If necessary, the addition of antipsychotics and benzodiazepines may be used, depending on the severity of episode.
If the first-line agent, at optimal doses, fails to produce significant clinical benefit, alternative strategies may include switching lithium to valproate or vice versa, or adding carbamazepine or oxcarbazepine in lieu of additional first-line medication, or adding antipsychotics if not already used.
Clozapine may be particularly effective in the treatment of refractory illness.
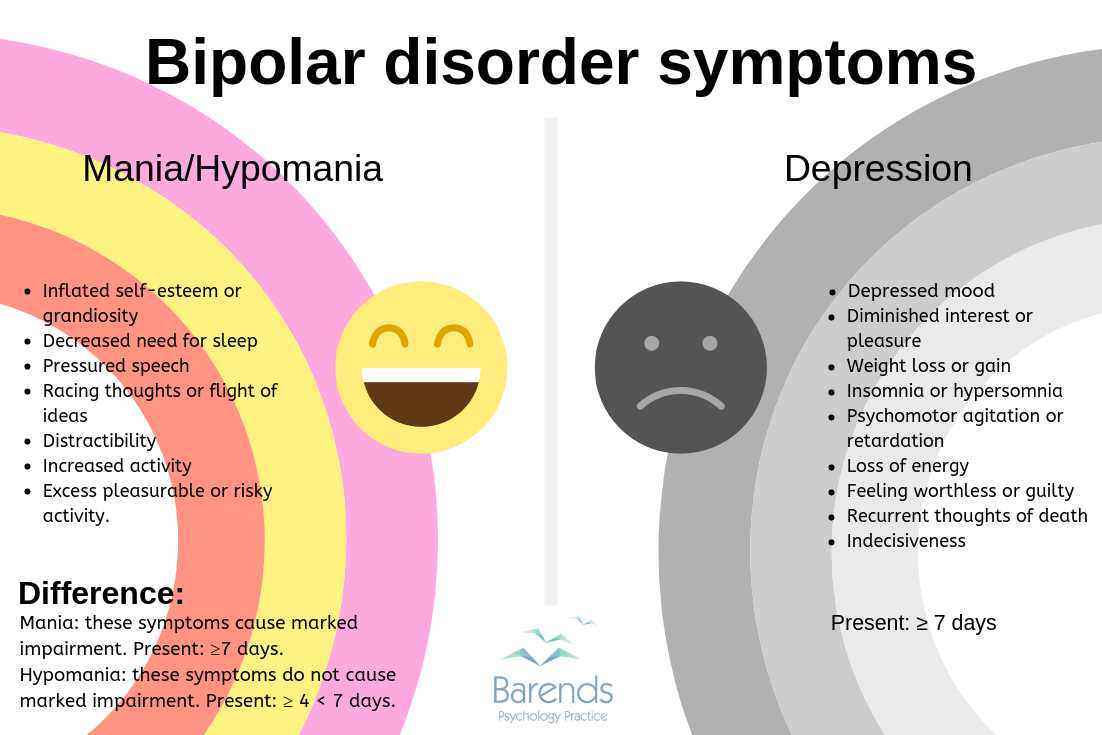
What Differentiates Bipolar 1 From Bipolar 2
While those with bipolar disorder all have disturbances in mood, psychologists differentiate between bipolar 1 and bipolar 2 disorders. Bipolar 1 disorder is when someone experiences a full manic episode at some point in their life, and may or may not experience depression. Bipolar 2 disorder is diagnosed in those with periods of depression and a lower grade of mania, called hypomania.
Even only having one full manic episode in your lifetime will be characterized as bipolar 1 disorder as compared to bipolar 2. Mania must last longer to be a full manic episode, one week or more hypomania only needs to occur for four days to be an episode and considered part of bipolar 2.
Someone with bipolar 1 will have experienced a manic episode, but it depends on the person whether they experience periods of depression. Usually, they will experience depression as well for at least two weeks, but the length can vary. There can also be a mix of depressive and manic symptoms at one time with bipolar 1.
You May Like: Definition Of A Phobia
What Should You Not Say To Someone With Bipolar
9 Things Not to Say to Someone Who Has Bipolar Disorder Youre Just Overreacting Again Anything That Doesnt Kill You Makes You Stronger Everybody Has Mood Swings Sometimes Everyone Is a Little Bipolar Sometimes You Are Psycho Youre Acting Like a Maniac I Wish I Was Manic so I Could Get Things Done.
What Are Bipolar Disorder Risk Factors
When someone develops bipolar disorder, it usually starts when they’re in late adolescence or young adulthood. Rarely, it can happen earlier in childhood. Bipolar disorder can run in families.
Men and women are equally likely to get it. Women are somewhat more likely than men to go through “rapid cycling,” which is having four or more distinct mood episodes within a year. Women also tend to spend more time depressed than men with bipolar disorder.
Bipolar disorder usually develops later in life for women, and theyâre more likely to have bipolar disorder II and be affected by seasonal mood changes.
A combination of medical and mental issues is also more common in women. Those medical issues can include thyroid disease, migraine, and anxiety disorders.
Some things that make you more likely to have bipolar disorder include:
-
Having a family member with bipolar disorder
-
Going through a time of high stress or trauma
-
Drug or alcohol abuse
-
Certain health conditions
Many people with the condition abuse alcohol or other drugs when manic or depressed. People with bipolar disorder are more likely to have seasonal depression, co-existing anxiety disorders, posttraumatic stress disorder, and obsessive-compulsive disorder.
Recommended Reading: Fear Of Spoons Phobia Name
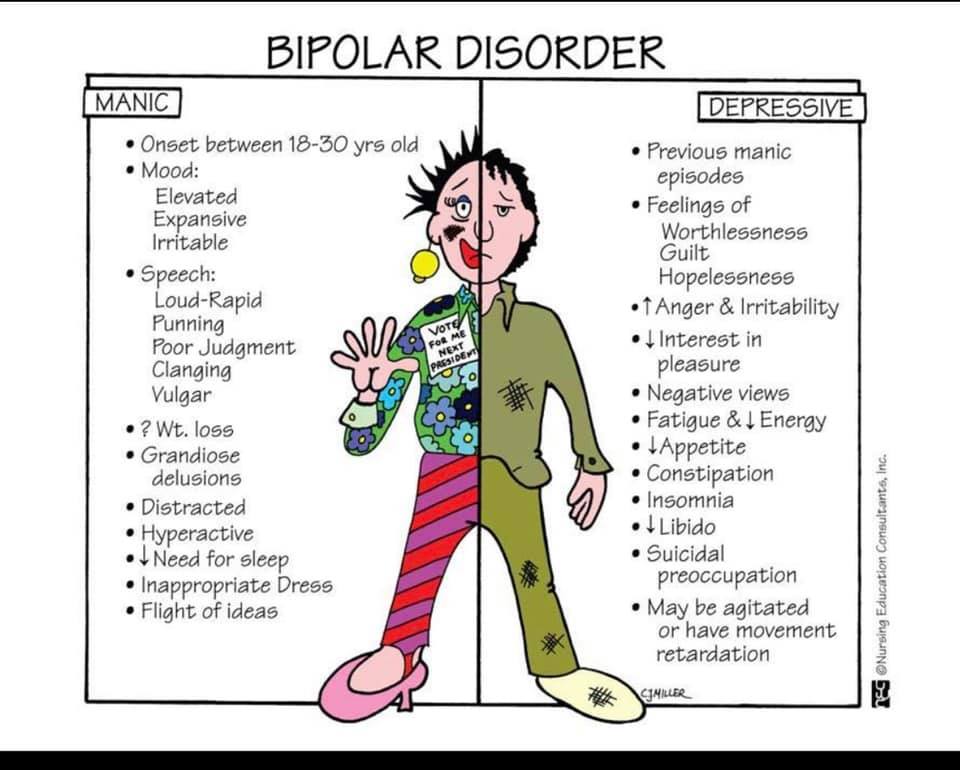
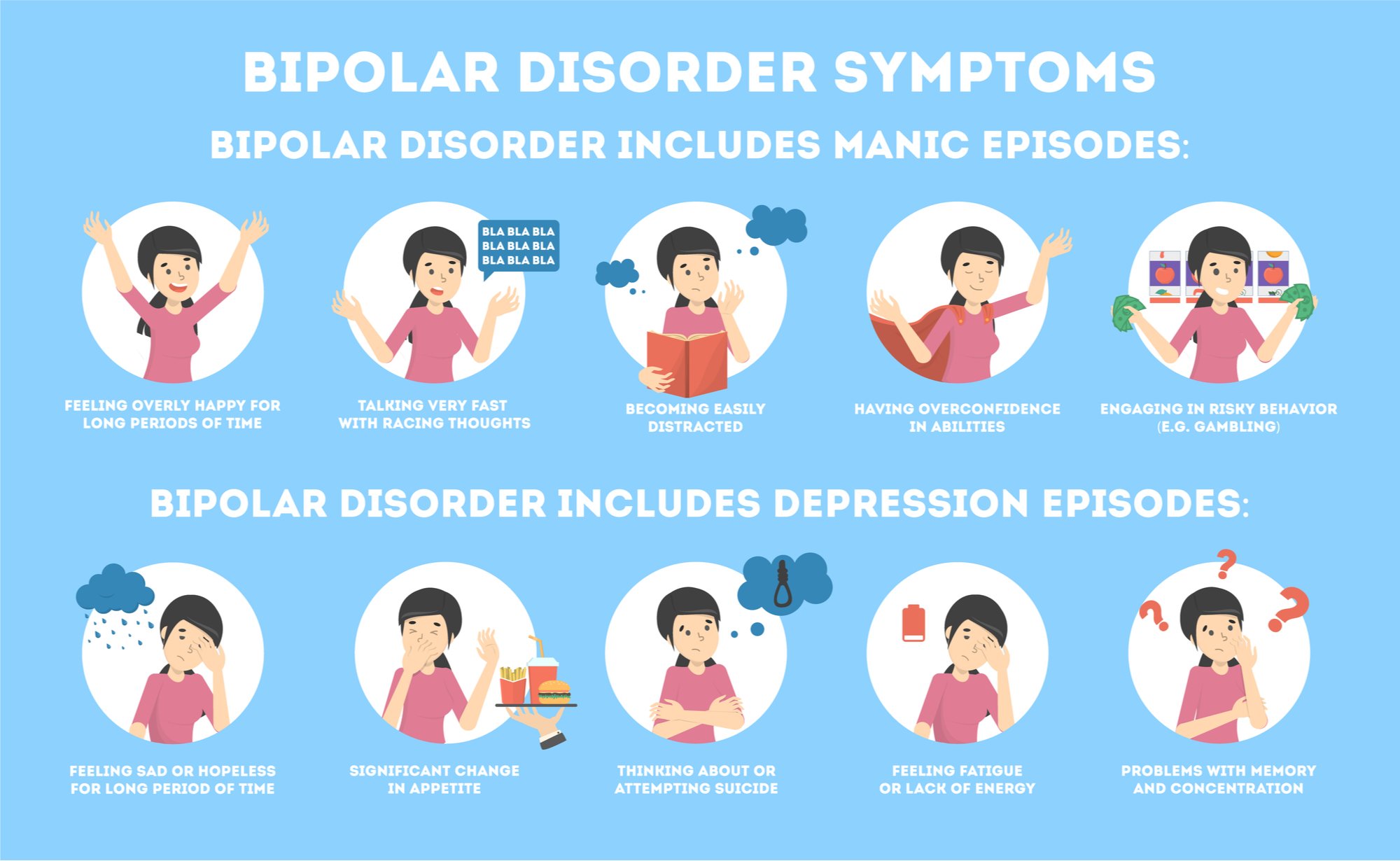
Symptoms Of Manic Episodes
Episodes of mania and hypomania are prevalent features of bipolar disorder. While the signs of mania may at first be a pleasant diversion from the dark depressive episodes, the manic phase can also be destabilizing and self-destructive.
Symptoms include:
- Racing thoughts and difficulty staying focused, easily distracted
- Rapid speech
- Impulsive behaviors, using poor judgment
- Risky behaviors, such as substance use or sexual promiscuity
- Psychosis
The Challenges Associated With Co
The definition of co-morbidity is the simultaneous presence of two or more conditions in one patient. Approximately 50 percent of individuals with bipolar disorders are co-morbid and are living with other psychiatric or medical conditions. Unfortunately, this can often make proper diagnosis and/or treatment more challenging. The following are some conditions that can impact the diagnosis and treatment of bipolar disorder:
Don’t Miss: Is Prozac Good For Panic Attacks
Can It Be Prevented
Once you begin to experience mood episodes, you can take steps to help reduce the severity of those episodes and lower your chances of experiencing additional mood episodes. But you cant always prevent mood episodes entirely or keep the condition from developing in the first place.
Future research may reveal more about the specific causes of bipolar disorder and give researchers more insight into potential ways of preventing the condition.
Bipolar Disorder And Relationships
Bipolar disorder can affect any of your relationships. But these effects might show up most clearly in your closest relationships, like those with family members and romantic partners.
When it comes to managing a relationship while living with bipolar disorder, honesty can always help. Being open about your condition can help your partner better understand your symptoms and how they can offer support.
You might consider starting with a few basic details, including:
- how long youve had the condition
- how episodes of depression usually affect you
- how episodes of mania usually affect you
- your treatment approach, including therapy, medication, and coping strategies
- anything they can do to help
Want more tips on maintaining a healthy relationship when you or a partner has bipolar disorder? Our guide can help.
Don’t Miss: How To Motivate Yourself To Workout When Depressed
Finding Treatment For Bipolar Disorders
If you or a loved one believe you may have bipolar disorder, please seek out a mental health professional for diagnosis and treatment. Look for a psychiatrist and licensed therapist with specialization in bipolar disorders. They will be able to help you and determine the best next steps.Knowing where to start when looking for providers can feel overwhelming, but Talkspace is here to help. Talkspace makes therapy accessible and affordable. If youre looking to take the first step consider finding a therapist or psychiatrist with Talkspace to get started today.
What Is Bipolar I Disorder Definitions Symptoms Treatment
Bipolar I disorder is a serious mental illness that affects hundreds-of-thousands of Americans every year. Bipolar I disorder affects approximately one percent of the population over the course of their lifetime in the United States. This equals three million people in the United States. To put that in perspective, thats slightly less than the risk of a woman developing bladder cancer in her lifetime or approximately equal to the risk of a man developing stomach cancer in his lifetime.
This type of bipolar disorder is often thought of as classic bipolar disorder as its symptoms were the first diagnostically recognized and its the kind most frequently portrayed in the media. Bipolar disorder type I is characterized by periods of a highly elevated or irritable mood known as mania alternating with periods of deep, profound depression. People with bipolar disorder type I can also experience periods without mood symptoms or with few mood symptoms. These are known as euthymic periods or euthymia.
You May Like: Feretrophobia Define
Symptoms Of Depressive Episodes
Depressive episodes can also emerge without warning. Some of the triggers for these depressive periods include lack of sleep, excessive stress, or a negative life event, but often there is no known cause for the depression. The depressive episodes must be carefully monitored, as there is an increased risk of suicidal behavior during these phases.
Symptoms include:
- Feelings of despair and hopelessness
- Intense fatigue
- Loss of interest in activities once enjoyed
- Chronic pain with no known medical cause
- Trouble concentrating
- Suicidal thoughts
Bipolar I Vs Bipolar Ii
Bipolar I disorder and bipolar II disorder are two of the three major forms of bipolar disorder. While both involve shifts in mood, energy, activity levels and concentration, BP-I and BP-II have two key differences. These differences include the intensity of manic episodes and the prevalence of major depressive episodes.
One major difference between BP-I and BP-II is the intensity of manic episodes. BP-I involves periods of severe mania whereas BP-II involves periods of less severe hypomania.
Mania and hypomania are both marked by persisting elevated, expansive or irritable mood that is uncharacteristic of the person at baseline. These periods may also involve abnormally elevated self-esteem, decreased need for sleep, increased talkativeness, flight of ideas or racing thoughts, abnormal distractibility, increased energy or goal-directed activity and abnormally risky behaviors.
Mania lasts for at least one week and is considered a medical emergency, often requiring psychiatric hospitalization. Its effects on ones personal life and ability to work are debilitating. Hypomania lasts for at least four days. It does not cause impairment in functioning, require hospitalization, or have psychotic features.
Recommended Reading: Feretaphobia
Risk Factors For Bipolar 1 Disorder
Bipolar disorder is more common in high-income countries than in low-income ones.
Research shows that the chances of bipolar 1 disorder increase by 10-fold if there is a family history of the illness.
Those chances increase further with closer relationships. For instance, if a biological mother or father had bipolar 1 disorder then the chances of getting diagnosed with the disorder are higher.
Bipolar Disorder: A Quick Diagnostic Review
The American Psychiatric Associations Diagnostic and Statistical Manual of Mental Disorders currently lists five types of bipolar and related disorders: bipolar 1, bipolar 2, cyclothymic disorder, other specified bipolar and related disorders, and unspecified bipolar and related disorders.
Bipolar 1 and 2 are the most common subtypes, with bipolar 1 disorder being more severe as to manic episodes.1 Both bipolar 1 and 2 disorder share many similarities, with the key differences being that bipolar 1 requires at least one manic episode, while bipolar 2 requires at least one hypomanic episode and at least one episode of major depressive disorder. Although major depressive episodes are common in patients with bipolar 1 disorder, it is not necessary for a type I diagnosis. See the full bipolar disorder DSM-5 diagnostic criteria.
The mean age of onset for bipolar 1 disorder is 18 years,1 and there is often a significant delay between the onset of symptoms and contact with mental health services. The lifetime prevalence of bipolar 1 disorder is estimated at 1% to 2.4% of the adult population, with occurrence rates similar between males and females. More on lifetime prevalence by sex and associated genetic and environmental risks for bipolar disorder.
Herein, we focus on current treatment recommendations for bipolar 1 disorder as derived from the American Psychiatric Associations most current practice guidelines,2,3 the DSM-5,1 and the literature.4-10
Don’t Miss: Depression On A Map