The Fine Line Between Remembering Too Much And Too Little
Posted March 18, 2011
What would it be like if we could remember everything that happens to us? Our lives would probably lose direction and meaning as was the case with S., the subject in A.R. Luria’s classic case history, The Mind of the Mmenonist. Mr. S. could recall details of all his experiences even years after their occurrence. Yet, he never focused on a particular goal or lasted long at a job or career. Instead, he ended up performing as a mnemonist, astonishing crowds with his powers of recall. However, the details he recollected were often meaningless lists of words. Significant and trivial experiences were remembered in equal measure.
A few weeks ago, I visited a friend who lives in Manhattan. Her apartment windows overlook the site of the former World Trade Center, and she described to me her experience of watching the towers come down. “I can see it and smell it like it was yesterday,” she said. That she remembered these events in such detail is not surprising to most of us. Emotionally charged events often produce our most powerful and intrusive memories.
S Of The Brain Impacted By Ptsd
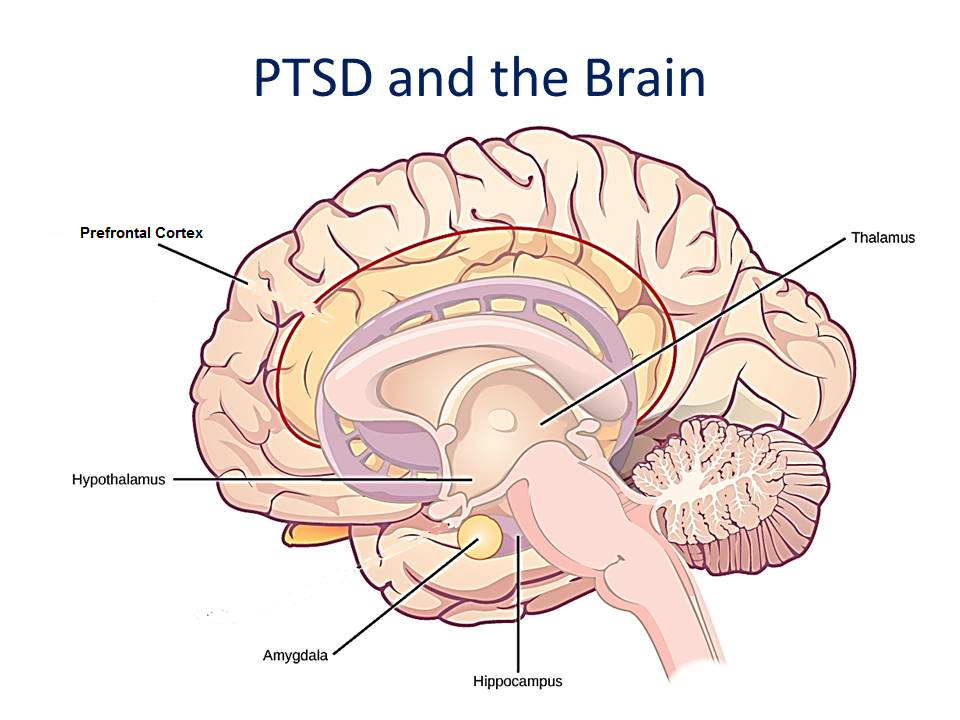
Certain structures of the brain are closely related to some of the symptoms of PTSD. These structures include the amygdala and hippocampus several parts of the prefrontal cortex the mid-anterior cingulate cortex and the right inferior frontal gyrus.
PTSD causes the hyper-activation of some brain structures while other areas become hypoactive.
Both the amygdala and the mid-anterior cingulate cortex become over-stimulated when a person has PTSD. However, the hippocampus, right inferior frontal gyrus, ventromedial PFC, dorsolateral PFC, and orbitofrontal cortex all become hypoactive, some to the point of atrophy.
How Ptsd Affects The Brain
If youre experiencing post-traumatic stress disorder , its important to understand how the different parts of your brain function. Post-traumatic stress is a normal response to traumatic events. However, PTSD is a more serious condition that impacts brain function, and it often results from traumas experienced during combat, disasters, or violence.
Your brain is equipped with an alarm system that normally helps ensure your survival. With PTSD, this system becomes overly sensitive and triggers easily. In turn, the parts of your brain responsible for thinking and memory stop functioning properly. When this occurs, its hard to separate safe events happening now from dangerous events that happened in the past.
Over the past 40 years, scientific methods of neuroimaging have enabled scientists to see that PTSD causes distinct biological changes in your brain. Not everybody with PTSD has exactly the same symptoms or the same brain changes, but there are observable patterns that can be understood and treated.
The diagram shows a cross-section of the brain parts discussed here.
Also Check: Can You Be Bipolar And Have Bpd
Cognitive Function And Brain Structure In Ptsd
Studies in PTSD are consistent with changes in cognition and brain structure. Multiple studies have demonstrated verbal declarative memory deficits in PTSD.,-
The meaning of findings related to deficits in memory and the hippocampus in PTSD, and questions related to the relative contribution of genetic and environmental factors, has become an important topic in the field of PTSD and stress research. There are three possible models, taking into account genetic or environmental factors, which have been proposed to explain smaller hippocampal volume in PTSD: Model A , Model B , and Model C .- In Model C , smaller hippocampal volume represents a premorbid risk factor for PTSD. In support of this model Pitman and colleagues have demonstrated that lower premilitary IQ is associated with combat-related PTSD, as well as finding a correlation between PTSD symptoms and hippocampal volume in twin brothers. Model A states that stress leads to damage or inhibition of neurogenesis via hypercortisolemia, decreased BDNF, or increased glutamate. Model B states that a combination of environmental and genetic factors leads to deficits in hippocampal function and structure. Showing that an intervention like medication changes hippocampal volume and cognition would provide support for at least a partial contribution of the environment to the outcomes of interest.
Is The Amygdala Bigger In People With Ptsd
The size of the right amygdala was 0.122 percent of total brain volume, on average, in the group with mTBI and PTSD. It was 0.115 percent in the cohort with only mTBI. The size of the left amygdala was 0.118 percent of brain volume in those with mTBI and PTSD, compared with 0.112 percent in the mTBI group.
Read Also: Dr Marilyn Vache
Why Choose Amen Clinics For Treating Ptsd
Most psychiatrists never look at the brain and can only make their assessment based on symptoms, which is why people often go undiagnosed or are misdiagnosed and given the wrong kind of treatment. Brain scans can be very helpful in getting a PTSD diagnosis. Two studies published by the research team at Amen Clinics showed that brain SPECT imaging is able to differentiate PTSD from TBI with a 94% accuracy rate. By comparison, MRI and CT scans often show normal results in people with PTSD, which makes them think they are imagining their symptoms. This research was recognized by Discover Magazine as #19 of the top 100 science stories of 2015. At Amen Clinics, a comprehensive evaluation that includes brain imaging paves the way for people with PTSD to get an accurate diagnosis and more effective treatment for faster healing.
Alcoholism And Binge Drinking
The amygdala appears to play a role in binge drinking, being damaged by repeated episodes of intoxication and withdrawal. Alcoholism is associated with dampened activation in brain networks responsible for emotional processing, including the amygdala.Protein kinase C-epsilon in the amygdala is important for regulating behavioral responses to morphine, ethanol, and controlling anxiety-like behavior. The protein is involved in controlling the function of other proteins and plays a role in development of the ability to consume a large amount of ethanol. The duration of chronic alcohol consumption and abstinence may affect dynamic brain network adaptations.
Read Also: Which Organization Sets The Standards For Diagnosing Eating Disorders
Emotional Trauma And The Amygdala
The amygdala is a section of nervous tissue in the brain that is responsible for emotions, survival instincts, and memory.
A major role of the amygdala is to detect fear. It recognizes and gathers information around us to determine threats. By using our senses, such as sight and sound, the amygdala will respond with the feeling of fear if it perceives a threat. This all happens unconsciously, deep in our brains.
When affected by PTSD, the amygdala becomes hyperactive.
Those who suffer from emotional trauma will often exhibit more fear of traumatic stressors than others. Often, stimuli can trigger overactivity in the amygdala if somehow connected to the traumatic event a person suffered from.
This might lead to chronic stress, heightened fear, and increased irritation. This might also make it harder for those suffering to calm down or even sleep.
Mri Assessment Of Brain Abnormalities In Ptsd And Trauma Spectrum Disorders
Findings of smaller hippocampal volume appear to be associated with a range of trauma related psychiatric disorders, as long as there is the presence of psychological trauma. We have used MRI to show smaller hippocampal volume in PTSD,,,, depression, depression with early abuse, borderline personality disorder with early abuse, and Dissociative Identity Disorder with early abuse. The greatest magnitude of difference was seen in the DID patients, who had unusually severe early childhood sexual abuse histories. We did not find changes in hippocampal volume in patients with panic disorder without a history of abuse . We found smaller amygdala volume in BPD with early abuse and increased amygdala volume in depression., Patients with depression had smaller orbitofrontal cortex volume with no changes in anterior cingulate or medial prefrontal cortex . More recently, we found smaller anterior cingulate volume in women with abuse and PTSD relative to controls.
Don’t Miss: When To Take Pristiq
Increased Inhibition Of The Amygdala By The Mpfc May Reflect A Resilience Factor In Post
- 1Department of Radiology, Hainan General Hospital, Haikou, China
- 2Department of Medical Imaging, Jinling Hospital, Medical School of Nanjing University, Nanjing, China
- 3Department of Neurology, Hainan General Hospital, Haikou, China
- 4Mental Health Institute, The Second Xiangya Hospital, National Technology Institute of Psychiatry, Key Laboratory of Psychiatry and Mental Health of Hunan Province, Central South University, Changsha, China
Purpose: To determine whether effective connectivity of the amygdala is altered in traumatized subjects with and without post-traumatic stress disorder .
Materials and Methods: Resting-state functional MRI data were obtained for 27 patients with typhoon-related PTSD, 33 trauma-exposed controls , and 30 healthy controls . Effective connectivity of the bilateral amygdala was examined with Granger causality analysis and then compared between groups by conducting an analysis of variance.
Trauma leads to an increased down-top excitation from the amygdala to the mPFC and less regulation of the amygdala by the dlPFC. The results suggest that increased inhibition of the amygdala by the mPFC may reflect a resilience factor, and altered amygdala-SMA and amygdala-STG effective connectivity may reflect compensatory mechanisms of brain function. These data raise the possibility that insufficient inhibition of the amygdala by the mPFC might lead to PTSD in those who have been exposed to traumatic incidents, and may inform future therapeutic interventions.
How Treatments Affect The Brains Of People With Ptsd
Some studies show that psychotherapies which include repeated exposure to trauma cues can enhance the ability of the PFC to assign less threatening or more positive meanings to trauma-related events. Antidepressants seem to have a similar effect. Mindfulness interventions lasting 10 to 12 weeks have been shown to decrease amygdala volume and increase the connectivity between the amygdala and PFC. Mindfulness seems to make the amygdala less reactive and the PFC more able to calm down the threat response. But some people with PTSD may have difficulty tolerating being mindful or confronting their trauma actively. Avoidance is a hallmark of PTSD and some patients may need more support and relationship-building before they are ready to face their distressing feelings.
Recommended Reading: Pristiq What Is It Used For
Does The Hippocampus Play A Role In Determining Ptsd Risk
Not everyone who experiences a traumatic event develops PTSD. Therefore, researchers have also proposed that the hippocampus may play a role in determining who is at risk for developing PTSD.
Specifically, it is possible that having a smaller hippocampus may be a sign that a person is vulnerable to developing a severe case of PTSD following a traumatic event. Some people may be born with a smaller hippocampus, which could interfere with their ability to recover from a traumatic experience, putting them at risk for developing PTSD.
In twin studies that focused on identical twins, with one twin exposed to a traumatic event and the other unexposed, researchers are able to look at pre-existing vulnerabilities that may be present in both twins, as well as differences that may be due to trauma. Since twin participants share the same genes, studying identical twins can provide insight into the influence of genetics on developing certain conditions.
For example, in this case, if the person who developed PTSD has a smaller hippocampus and has a non-trauma exposed twin who has a smaller hippocampus, it would suggest that a smaller hippocampus may be a sign of genetic vulnerability for developing PTSD following a traumatic experience.
Introduction: Posttraumatic Stress Disorder
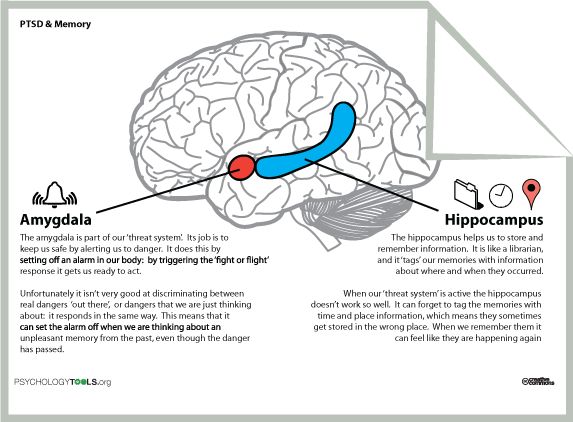
Figure 1.
Fear neurocircuitry model of PTSD . The ventral ACC and ventromedial prefrontal cortex are proposed to inhibit activity in the amygdala, and this top-down control is thought to be diminished in PTSD, leading to enhanced fear conditioning and poor fear extinction. PTSD, posttraumatic stress disorder vACC, ventral anterior cingulate cortex.
You May Like: Schizophrenic Subtypes
Functional Consequences Of Amygdala Hyporeactivity And/or Hyperactivity In Ptsd
Both amygdala hyperactivity and a failure to activate the amygdala appear to be outcomes associated with PTSD, with the direction of activity dependent upon biological and stimulus factors and symptom features. Therefore, it is important to consider the functional consequences and implications of either outcome for individuals with PTSD.
Figure 3.
Refined neurocircuitry model of PTSD . Symptoms of emotional disengagement and dissociative PTSD are thought to be associated with reduced amygdala reactivity to emotional stimuli, due to increased top-down control from the medial prefrontal cortex and dorsal ACC. In contrast, hyperarousal, hypervigilance, and deficits in fear conditioning and extinction are thought to arise in part from a hyperactive amygdala, due to diminished top-down control from the ventral ACC and ventromedial prefrontal cortex are proposed. dACC, dorsal anterior cingulate cortex PTSD, posttraumatic stress disorder vACC = ventral anterior cingulate cortex.
My Boss Wants Me To Go Back Into The Tank To Weld But Im Still Trying To Get Out
Joe
Joes brain has been hijacked by trauma. He feels out of control because he cant make his mind do what he wants it to do, which is to forget the trauma.
But despite what reason says, Joes body still holds on to the distress of the accident and is desperately trying to get out of the tank. The hijacking results in posttraumatic stress disorder . Some common symptoms of PTSD include nightmares, flashbacks, panic attacks, startle response, and preoccupation with the traumatic event.
How exactly are Joes brain and body being hijacked by the trauma? Simply put, when a person experiences something traumatic, adrenalin and other neurochemicals rush to the brain and print a picture there. The traumatic memory loops in the emotional side of the brain, disconnecting from the part of the brain that conducts reasoning and cognitive processing. The reasonable part of the brain is unable to help the emotionally loaded part of the brain get away from the trauma.
It is estimated that of 100 people who have experienced trauma, 25%, or 1 in 4, will experience PTSD, which includes 1 of every 4 burn survivors. With statistics this high, we can conclude that this is a normal response to an extreme situation and not a pathology.
UNDERSTANDING THE BRAIN AND BODY IN TRAUMA
Recommended Reading: Does Bipolar Disorder Get Worse With Age
Consequences Of Brain Dysfunctions In Ptsd
Hyperarousal
Because the amygdala is overactive, more norepinephrine is released in response to threat and its release is not well-regulated by the PFC.
Effects of excess norepinephrine include:
As a result of hyperarousal, people with PTSD can get emotionally triggered by anything that resembles the original trauma . Symptoms of hypervigilance means they are frequently keyed up and on edge, while increased wakefulness means they may have difficulty sleeping or wake up in the middle of the night.
How Does Trauma Affect The Brain
When we experience a traumatic event, our brain chemistry and functioning changes in response to the emotional and physical consequences of that event.
Traumatic events include a wide range of experiences, including:
- Physical or sexual abuse
- Death of a loved one
- Financial, professional, or personal loss
There is no standard definition of a traumatic experience for everyone, and each of these experiences takes a unique toll on us as individuals. While all of us experience traumatic stress in different ways, our brains process stress in mostly predictable patterns. In general, there are three major areas of our brain that are shaped by stressful experiences. These are:
- The hippocampus, which helps control memory, learning, and interpretation of information. This area of the brain may become less active under stress and, in fact, may actually shrink. This shrinkage reduces the amount of information and memories we can effectively process at one time. In addition, a smaller and less active hippocampus means we are less likely to be able to process any new information when we are experiencing traumatic stress.
- The amygdala, which helps us process our emotions. During periods of intense stress, the amygdalas role in the brain is to serve as an alarm system, alerting the rest of the brain to potential risk. While this is useful in life-or-death situations, the amygdala can be triggered by traumatic stress, too, causing the brain to enter fight-or-flight mode over and over again.
You May Like: Can Dehydration Cause Panic Attacks
Ptsd Symptom Load Assessments
At site 1, PTSD symptom scores were assessed using the MINI 6.0.0. The MINI is a short diagnostic structured interview that explores psychiatric diagnosis according to the DSM-IV and ICD-10. Each question has only two response options . The PTSD diagnostic section started out by using three screening questions , and if answered positively, 12 follow-up questions were asked in order to examine the presence of symptoms needed to fulfill the diagnostic criteria. PTSD load was calculated based on the number of positively answered questions for the PTSD diagnostic section . At site 2, subjects completed the PCL-C, which is a DSM-IV based 17-item rating scale with self-report ratings ranging from 1 to 5 for each item. At site 3, post-traumatic stress reactions were measured using the PTSD-RI. The PTSD-RI is a DSM-IV based 20-item scale in which responses are recorded on a 5-point scale, ranging from 0 to 4 . Since three of the items have two alternative formulation, only the formation leading to the highest score was utilized, resulting in 17 items being used for the total symptom scale score calculation. The PTSD symptom scores were z-standardized within each site before entering any analyses.
Can The Brain Heal Itself After Trauma
When evaluating the damage that emotional trauma and PTSD have caused, scientists have found that the brain is unable to heal itself. While the brain is unable to fully recover itself, Highland Springs is able to offer treatments to help prevent further damage and encourage healing for emotional trauma. With the experts that Highland Springs is able to offer, patients will be able to identify the cause of their trauma/triggers and eventually be able to overcome it.
Also Check: What Is The Phobia For Bees