How Is Anxiety Different Than Ptsd
When the average person hears anxiety, we start thinking pre-existing issues like Generalized Anxiety Disorder among others. Unlike PTSD, traumatic events dont necessarily have to happen for a person to experience anxiety symptoms. The difference between PTSD and anxiety can be tricky to pinpoint, especially when soldiers with history of mental health issues like anxiety are then exposed to extremely traumatic experiences in their military service. Their symptoms may be re-aggravated or made worse. Because every person is different and reacts differently to situations based on their coping skills, morals, values, and experiences in life reactions to those events will be different as well. Where one person may not have any lasting mental health condition to an event, another may develop PTSD. We do not know what causes one person to develop certain conditions and others to not, but we continue to try to understand and treat them.
Arousal And Reactivity Symptoms
Arousal and reactivity symptoms can look like hypervigilance or an exceptionally sensitive startle reflex. Common everyday noises, like a car door slamming, can make you jump out of your skin convince you that you are in immediate danger.
Hypervigilance can make it difficult to concentrate or sleep. This can lead to feelings of frustration and anger, which can worsen the symptoms of PTSD even further. Feeling jumpy and ill-at-ease all the time is exhausting and can be very disheartening and depressing.
Many people with high levels of reactivity symptoms turn to alcohol and other drugs in order to numb their senses and feel less reactive to the world around them.
Depression Or Major Depressive Disorder
Depression and PTSD often occur simultaneously. While current statistics on the link between the two are lacking, the National Center for PTSD cites a 1995 study that depression is about three to five times more likely in people who have PTSD than in those who dont.
Depression is widespread and is more serious than just feeling down on one particular day. Annually this mental illness affects an estimated 16 million American adults, and about one in every six adults in the United States will experience depression at some point in their lifetime .
Major depressive disorder, or clinical depression, seriously impedes your ability to function in everyday life. Its a mood disorder that can show itself in the form of having feelings of sadness and hopelessness, trouble sleeping, anxiety, or recurring thoughts of death and suicide, among other symptoms.
In many instances, depression can follow trauma. One example of a depression-inducing trauma is the Oklahoma City bombing in 1995 a domestic terror attack that resulted in 168 deaths, including 19 children . After the tragedy, 23 percent of survivors experienced depression. Before the bombing, just 13 percent of this same group of people reported having depression.
Don’t Miss: Prodromal Definition Psychology
Is Topiramate Prescribed All Over The World
Yes, many nations have approved Topiramate for use and prescribe it.
This information is not designed to replace a physician’s independent judgment about the appropriateness or risks of a procedure for a given patient. Always consult your doctor about your medical conditions. Remedy Health Media & PsyCom do not provide medical advice, diagnosis or treatment. Use of this website is conditional upon your acceptance of our User Agreement.
What Is Complex Ptsd

Complex post-traumatic stress disorder is a condition where you experience some symptoms of PTSD along with some additional symptoms, such as:
- difficulty controlling your emotions
- feeling very angry or distrustful towards the world
- constant feelings of emptiness or hopelessness
- feeling as if you are permanently damaged or worthless
- feeling as if you are completely different to other people
- feeling like nobody can understand what happened to you
- avoiding friendships and relationships, or finding them very difficult
- often experiencing dissociative symptoms such as depersonalisation or derealisation
- physical symptoms, such as headaches, dizziness, chest pains and stomach aches
- regular suicidal feelings.
You May Like: Pheritriphobia
Joint Features Of Multiple Conditions
The scientists searched for brain regions that were either more active or less active in the participants with mental health conditions than among the control group. As expected, the researchers found that certain features of brain activity were consistent across mood disorders, PTSD, and anxiety disorders.
Perhaps surprisingly, they found the most significant differences between the two groups of participants when they searched for hypoactive regions. The authors outline their primary findings:
detected statistically robust transdiagnostic clusters of hypoactivation in the inferior prefrontal cortex/insula, the inferior parietal lobule, and the putamen.
These regions are significant because they are all involved in emotional and cognitive control. Specifically, they play an important role in stopping cognitive and behavioral processes and switching to new ones.
Senior author Dr. Sophia Frangou explains: These brain imaging findings provide a science-based explanation as to why patients with mood and anxiety disorders seem to be locked in to negative mood states. They also corroborate the patients experience of being unable to stop and switch away from negative thoughts and feelings.
The authors also outline how these findings lend support to earlier studies in people with these disorders, which found deficits of large effect size in stopping and shifting responses in a range of tasks.
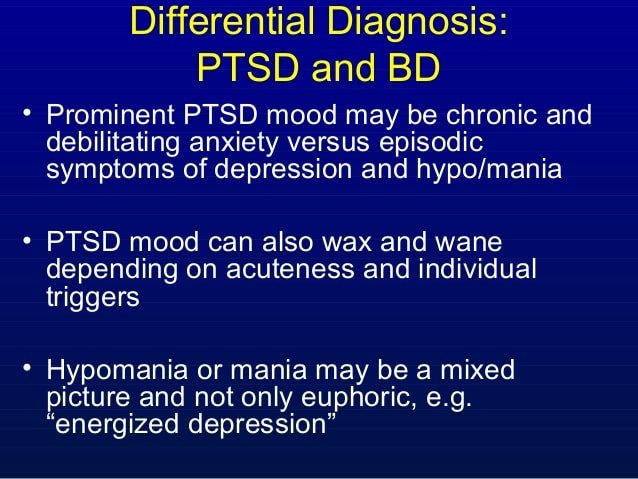
Traumas Impact On Bipolar Symptoms
The interactions between these two conditions are complicated and impossible to fully understand. However, if you already have bipolar disorder and then go through sustained trauma and develop C-PTSD, the results are likely to be more severe bipolar symptoms.
C-PTSD causes symptoms that affect mood. These can worsen your bipolar moods and cycles, especially if left untreated. Many of the symptoms unique to C-PTSD as compared to PTSD are similar to those of bipolar disorder.
As one example, during manic episodes you may feel edgy, tense, keyed up, and even angry or irritable. C-PTSD causes similar feelings and reactions. During mania, these symptoms may become additive, making you feel even worse and leading you to act out in even more destructive ways.
Both conditions can also cause symptoms characteristic of psychosis, such as dissociation or delusions. If you have both mental illnesses, you may be more likely to experience these severe and distressing symptoms.
Read Also: Is Tequila A Stimulant Or Depressant
Can You Have Both Ptsd And Bipolar Disorder
Its possible to have both conditions and many people do.
As noted above, evidence suggests that PTSD can increase your chances of developing bipolar disorder, while bipolar disorder could indirectly increase your chances of facing a traumatic experience.
Additional research supports the idea that either condition can contribute to the other.
One explored the rates of PTSD in 212 people diagnosed with bipolar disorder who were receiving inpatient care. Just over 72 percent of the participants had experienced some kind of trauma, while over 35 percent had a diagnosis of PTSD.
According to a
- Between 4 and 40 percent of people living with bipolar disorder also met criteria for PTSD.
- PTSD appeared more common in women and people living with bipolar I.
- Between 6 and 55 percent of people living with PTSD also met criteria for bipolar disorder.
- People living with both conditions tended to report worse symptoms and lower quality of life.
Older research notes that PTSD occurs, on average, in about 16 percent of people with bipolar disorder, compared to just under 8 percent of the general population.
If you do have both conditions, getting treatment for one might ease some of your symptoms but it generally wont improve them all.
Keep in mind that some treatments could worsen your symptoms. Antidepressants, which can help treat depression symptoms in PTSD, may sometimes trigger mania when used without a mood stabilizer, for example.
Ptsd And Risk For Social Anxiety Disorder
The symptoms of PTSD may make a person feel different, as though they can’t relate or connect with others. In addition, many people with PTSD feel high levels of depression, shame, guilt, and self-blame.
Therefore, it is not surprising that PTSD and social anxiety disorder frequently co-occur. Fortunately, there are very effective treatments available for both PTSD and social anxiety disorder. Learn more about the diagnosis of social anxiety disorder, its connection with PTSD and how one can get help for both conditions.
Don’t Miss: What Is A Phobia Of Spoons Called
Managing Symptoms Of Ptsd
PTSD is a diagnosable condition that requires professional treatment. Never try and treat yourself, or forgo treatment for something so serious.
There are things you can focus on in your everyday life to make treating your PTSD a little less painful make your life more bearable and healthier for yourself and the people who care about you.
Bipolar Disorder And Ptsd
A review published in 2017 concluded that up to 40% of people with bipolar disorder also meet criteria for PTSD. It is not entirely surprising that high rates of PTSD are found among people with bipolar disorder, as many people with bipolar also have a history of traumatic exposure.
Traumatic exposure may be more likely to occur during a manic episode when a person with bipolar disorder is more likely to make risky or impulsive decisions.
In addition to being a risk factor for the development of PTSD, traumatic exposure during childhood, such as childhood physical or sexual abuse, may also be risk factors for the development of bipolar disorder.
Don’t Miss: Feretrophobia
If Topiramate Has So Little Evidence Supporting Its Use Why Should Anyone Prescribe It Over An Older Drug That Has More Research Showing Its Effectiveness
First of all, Topiramate generally has a better side effect profile than those older drugs. Some patients find that older mood stabilizers have side effects that are too dangerous or impact their lives too much.Second of all, many patients find that the older drugs do not control their disorders, while Topiramate does. That makes it the only effective known remedy for them.Lastly, topirmate is so far the only psychopharmacologic agent that appears to have an effect in providing relief for PTSD symptoms. These symptoms can be extremely debilitating.
Trauma Is The Underlying Factor
When mental illnesses co-occur, it isnt possible to say with certainty that one caused the other or to outline exact reasons for the diagnoses. However, it is likely there are risk factors in common. These risk factors contribute to the onset of mental illness and make it more likely that an individual will get more than one diagnosis.
In the case of C-PTSD with bipolar disorder, trauma is the common contributing cause. Traumatic experiences over a long period of time do not ensure that you will develop either of these mental illnesses, but it significantly increases the risk.
Also Check: Does Pristiq Help With Anxiety
Why Bipolar Disorder Is Often Misdiagnosed
For some people with a history of mental illness, like the hypothetical Jane Grey, receiving a PTSD diagnosis may come as a shock. But these comorbidities are actually common and research suggests that a preexisting mental illness, such as major depressive disorder or bipolar disorder, may be a risk factor for PTSD.
If you or a loved one is dealing with PTSD and another mental illness, heres an overview of how to manage six conditions that commonly occur with PTSD.
Biological Factors That Distinguish Between Ptsd And Mdd
In contrast to the risk factor research described above, biological studies that address PTSD/MDD comorbidity generally examine how PTSD and MDD have distinct, and sometimes diverging, biological signals. This research includes studies that examine structural and functional neuroimaging, measures of the hypothalamic pituitary adrenal axis, and more recently, DNA molecular markers .
Recommended Reading: Does Celine Dion Have An Eating Disorder
Treatment For Complex Ptsd
Complex PTSD can be treated with the same strategies as PTSD, but many experts believe that care has to go beyond this and focus on helping victims re-establish control, power, and self-identity. This can be done through therapy, empowering activities, and healthful, supportive and safe relationships.
PTSD treatments that can help patients with complex PTSD include trauma-focused therapies. Exposure therapy, for instance, helps patients process trauma by facing the memories of it in a safe space and practicing healthy coping mechanisms. Eye movement desensitization and reprocessing uses eye movements guided by the therapist to process traumatic memories, reframe them, and change negative reactions to them.
Standard behavioral therapies can also help PTSD and C-PTSD patients. Behavioral therapists teach coping mechanisms, help patients recognize and change their negative thoughts, and teach patients how to be mindful and to address symptoms and feelings as they arise.
C-PTSD patients may also benefit from medications, although there are none that are specifically approved to treat PTSD. Anti-anxiety medications, antipsychotics, and antidepressants can help manage specific symptoms or co-occurring disorders that patients struggle with alongside or because of the C-PTSD.
The Dorsal Raphe Nucleus
While glucocorticoid release is necessary, but not sufficient, to produce LH, the behavioral changes associated with LH are critically dependent on the activation of serotonin cells in the caudal aspect of the dorsal raphe nucleus . The DRN is the primary 5-HT source to the forebrain and has been argued to be topographically organized such that the activation of different DRN subregions mediate different functions , with the caudal aspect mediating anxiety-associated behavioral states. Inescapable, relative to escapable, shock activates 5-HT neurons in the caudal region of the DRN , and this activation is associated with a significant increase in 5-HT release both in the DRN and its projection regions . The attenuation of DRN 5-HT activity via intra-DRN infusion of benzodiazepines , or the 5-HT1A autoreceptor agonist 8-OH-DPAT, blocks both the development and expression of LH . Also, pharmacologically activating 5-HT neurons in the caudal, but not rostral, DRN produces LH-like behavioral changes 24-hr later . Based on these data, Maier and colleagues have suggested that elevated 5-HT sensitizes the caudal DRN for a period of time after treatment, and that caudal DRN 5-HT sensitization mediates the behavioral effects of LH . While substantial evidence suggests caudal DRN 5-HT activation mediates LH, the input that activate the DRN during inescapable shock are not well understood.
You May Like: Psychology Behind Eating Disorders
What We Learned About Ptsd In Veterans
Post-traumatic stress disorder is complicated and overwhelming. It requires treatment and attention. However, it does not have to define you, and you dont have to suffer for the rest of your life. More and more research and understanding of PTSD comes out every day, and the stigma of mental health issues is fading rapidly.
If you or someone you care for has PTSD or you suspect that they may have PTSD, dont wait to ask for help. The sooner you start addressing the trauma you survived, the sooner you can begin to thrive again. There is help, there is hope, and there is recovery.
What Connects Depression Anxiety And Ptsd
In the largest study of its kind, researchers identify similarities in the brain activity of people with major depressive disorder, post-traumatic stress disorder, bipolar disorder, and anxiety disorders.
Mental health disorders, although incredibly prevalent, remain poorly understood.
According to the National Institute of Mental Health, almost 1 in 5 adults in the United States live with a mental illness.
About half of the U.S. population will experience a mental health condition at some point in their life.
Medication and talking therapies are useful for many people, but understanding the neurological roots of these conditions is proving challenging.
You May Like: What Does A Ptsd Flashback Look Like
How Is Depression Different From Ptsd
Depressive disorders are also similar to PTSD in the symptomology and often in etiology. For our blog on PTSD and depression click here. Depression is not just being moody or sad. Depression is a serious illness where the depressive state can last months or even years and only treatment like psychiatry and psychotherapy can help. A person cannot just snap out of it. Depressive disorders can be caused by the same traumatic events that cause PTSD, as well as difficult life circumstance, medical conditions, grief, and stress. Differentiating between depression and PTSD can be challenging but it can also be a bit more straightforward than trying to do so for anxiety and PTSD. This is because many of the symptoms PTSD and Anxiety share are not typically seen with depression such as vivid flashbacks and hyperawareness. Lets check out the most common depressive disorders and symptoms below.
What Does The Research Say
Research from 2016 reviewed multiple studies exploring the link between bipolar disorder and childhood trauma. Researchers concluded that trauma didnt just increase bipolar disorder risk. It also seemed to lead to more severe symptoms, including suicidal thoughts or attempts.
In a nationwide study from 2016 , researchers used the Danish Civil Registration System to explore potential links between bipolar disorder, schizophrenia spectrum disorders, and a diagnosis of PTSD or acute stress reaction.
Their findings suggest that people diagnosed with traumatic stress had a higher risk of developing bipolar disorder or schizophrenia spectrum disorders. This risk seemed to be highest during the first year following a traumatic stress diagnosis, but it stayed high for over 5 years. Researchers also noted that the link didnt relate to a family history of either condition.
Of course, as other research points out, the link could run in the other direction, too. People often feel more impulsive than usual during manic episodes. This impulsivity can lead you to take risks that might put you in danger or cause other harm, such as:
- driving too fast
- trying an extreme sport with taking safety precautions
- getting in a fight with your boss
These experiences can cause lasting trauma when they have a negative outcome, for you or anyone else.
Also Check: What Makes Tequila A Stimulant