Schizophrenia Is It The Same As Multiple Personality Disorder
Dr. Lieberman explains if schizophrenia is the same as multiple personality disorder.
Dr. Lieberman:There are many misconceptions about what schizophrenia is and isnt, and maybe the biggest is that it does not mean split or multiple personality. Thats completely wrong, and its just sort of out there in our culture unfortunately, and somebody says, Oh, when you act one way one time and another way another time, oh, you are acting schizophrenic, thats completely untrue.
Multiple personality is something thats very rare and does not involve delusions, hallucinations, thought disorganization, negative symptoms, cognitive impairment, all of the cardinal signs of schizophrenia.
Schizophrenia: The 7 Keys To Self
Seek social support. Friends and family vital to helping you get the right treatment and keeping your symptoms under control. Regularly connecting with others face-to-face is also the most effective way to calm your nervous system and relieve stress. Stay involved with others by continuing your work or education. If thats not possible, consider , joining a schizophrenia support group, or taking a class or joining a club to spend time with people who have common interests. As well as keeping you socially connected, it can help you feel good about yourself.
Manage stress. High levels of stress are believed to trigger schizophrenic episodes by increasing the bodys production of the hormone cortisol. As well as staying socially connected, there are plenty of steps you can take to reduce your stress levels. Try adopting a regular relaxation practice such as yoga, deep breathing, or .
Get regular exercise. As well as all the emotional and physical benefits, exercise may help reduce symptoms of schizophrenia, improve your focus and energy, and help you feel calmer. Aim for 30 minutes of activity on most days, or if its easier, three 10-minute sessions. Try rhythmic exercise that engages both your arms and legs, such as walking, running, swimming, or dancing.
How Is Dissociative Identity Disorder Diagnosed
Making the diagnosis of dissociative identity disorder takes time. Its estimated that individuals with dissociative disorders have spent seven years in the mental health system prior to accurate diagnosis. This is common, because the list of symptoms that cause a person with a dissociative disorder to seek treatment is very similar to those of many other psychiatric diagnoses. In fact, many people who have dissociative disorders also have coexisting diagnoses of borderline or other personality disorders, , and .
The DSM-5 provides the following criteria to diagnose dissociative identity disorder:
Recommended Reading: Prodromal Symptoms Of Schizophrenia Are Evident
Why Is Dissociative Identity Disorder Confused With Schizophrenia
The main reasons why people confuse dissociative identity disorder with schizophrenia include:
- Certain symptoms overlap in both conditions.
- Dissociation from reality is misinterpreted by many as the presence of multiple personalities.
- The popular culture portrayals in novels and films lead people to believe that every hallucinating patient has schizophrenia.
However, DID often originates as a coping mechanism to an extremely traumatic episode in childhood, whereas schizophrenia is more likely to be genetic in origin with additional environmental factors at play.
The following symptoms may overlap in DID and schizophrenia confusing diagnosis:
- Hallucinations
- Memory issues
Are Schizophrenics Highly Intelligent

Schizophrenia patients are typically found to have low IQ both pre- and post-onset, in comparison to the general population. However, a subgroup of patients displays above average IQ pre-onset. The nature of these patients illness and its relationship to typical schizophrenia is not well understood.
Read Also: Phases Of Schizophrenia
Dissociative Model In Patients With Resistant Schizophrenia
- Psychiatric Clinic, University Hospital for Active Treatment Prof. D-R Stoian Kirkovic, Trakia University, Stara Zagora, Bulgaria
Background: Schizophrenia is a severe mental illness in which, despite the growing number of antipsychotics from 30 to 50% of patients remain resistant to treatment. Many resistance factors have been identified. Dissociation as a clinical phenomenon is associated with a loss of integrity between memories and perceptions of reality. Dissociative symptoms have also been found in patients with schizophrenia of varying severity. The established dispersion of the degree of dissociation in patients with schizophrenia gave us reason to look for the connection between the degree of dissociation and resistance to therapy.
Methods: The type of study is correlation analysis. 106 patients with schizophrenia were evaluated. Of these, 45 with resistant schizophrenia and 60 with clinical remission. The Positive and Negative Syndrome Scale and Brief Psychiatric Rating Scale scales were used to assess clinical symptoms. The assessment of dissociative symptoms was made with the scale for dissociative experiences . Statistical methods were used to analyze the differences in results between the two groups of patients.
The level of dissociation measured in patients with resistant schizophrenia is as high as the points on the DES in dissociative personality disorder.
Symptoms Of Dissociation In Ssds
Several studies examined symptoms of dissociation in schizophrenia spectrum patients through the Dissociative Experiences Scale , which is the most commonly used instrument for measuring dissociation. The questionnaire contains 28 items describing dissociative experiences. The respondent is asked to state how often they had each experience ranging from 0% to 100% of the time, resulting in mean scores ranging from 0 to 100. Mean scores for healthy controls ranged between 4.38 and 14.86, whereas mean scores of patients with a DD ranged between 24.9 for depersonalization disorder and 57.06 for multiple personality disorder .
Also Check: Charles Manson Mental Diagnosis
What Kind Of Symptoms Might People With Schizophrenia Have
People with schizophrenia may have a number of psychotic symptoms. These symptoms can come and go in phases, or they can happen only once or twice in a lifetime. When the illness begins, psychotic symptoms are usually sudden and severe.
During psychotic phases, the person may still understand parts of reality. He or she may lead a somewhat normal life, doing basic activities such as eating, working and getting around. In other cases, the person may be unable to function. Symptoms during psychotic phases include:
- Seeing, hearing, feeling or smelling things that are not real .
- Having strange beliefs that are not based on facts . For example, the person may believe that people can hear his or her thoughts, that he or she is God or the devil, or that people are putting thoughts into his or her head.
- Thinking in a confused way, being unable to make order out of the world, shifting quickly from one thought to the next.
- Having emotions, thoughts and moods that do not fit with events.
People with schizophrenia also may:
- Have a lot of energy or be overly active, or become “catatonic,” a state in which the body becomes rigid and cannot be moved.
- Talk in sentences that do not make sense.
- Not wash or groom.
- Cut themselves off from family, friends and the outside world.
- Be unable to function in school, work, or other activities.
- Lose interest in life.
- Be very sad or have mood swings.
- Have dulled emotions.
The Causes Aren’t Crystal Clear For Either Disorder
People develop the conditions at different stages in life. With schizophrenia, someone will have a break in their early 20s if they are a man, and in their mid to late 20s if they are a woman. With DID, it tends to be a much more gradual thing that happens from childhood, before the age of about 7.
Having a troubled past puts people at a higher risk for developing schizophrenia in their lifetime, but this connection is not well understood yet.
Over the years, there has been research suggesting schizophrenia is biological, or genetic, and thus is inherited. Muller said that during his undergraduate degree in the 1980s he was taught something called the dopamine hypothesis that backs this up, but in the years since, there has been insufficient data on this line of thinking.
Other studies have shown there is an increased risk of developing schizophrenia if you are an identical twin and they have the disorder, suggesting a genetic element. However, as Muller pointed out, if your identical twin has anything like a penchant for spicy food you are more likely to have that too, and this could be down to any number of different factors of nature and nurture.
Muller said every decade or so there is a new theory that is taught to psychiatric students until the next one comes along, such as the idea that schizophrenia is related to brain ventricles. However, it’s still very unclear of what the causes really are.
Recommended Reading: Define Phobia Disorder
People With Did Have Been Through Terrible Psychological Trauma
Muller said in almost every case, the patient has been through severe childhood trauma.
Several studies have shown the connection with childhood trauma and dissociation, including the work of Dr Bethany Brand, who looked into police records and found that people with DID had all routinely had severe violence or abuse in their childhood.
“These individuals almost always have severe physical, sexual, or psychological abuse from the caregiver,” said Muller. “In fact, it’s almost impossible to find a case of someone with DID who hasn’t had that.”
The individual has had a profound violation of trust or betrayal, he said, “a father or mother who has raped them, or sold them into prostitution at a young age, or another of the horrific things that happen to people.”
The only way to cope with the traumatic experience is to shut off from the outside world. The individual goes into an altered state of consciousness as a way of coping a bit like an immune response. The brain knows something is incredibly difficult to deal with and shuts off its awareness of the situation as a way of protecting itself.
Schizophrenia: Early Warning Signs
Early detection and treatment of conditions such as heart disease and cancer have improved survival rates and quality of life for people who suffer from these conditions. A new approach involves identifying people who show minor symptoms of psychosis, such as unusual thought content, paranoia, odd communication, delusions, problems at school or work, and a decline in social functioningwhich are coined prodromal symptomsand following these individuals over time to determine which of them develop a psychotic disorder and which factors best predict such a disorder. A number of factors have been identified that predict a greater likelihood that prodromal individuals will develop a psychotic disorder: genetic risk , recent deterioration in functioning, high levels of unusual thought content, high levels of suspicion or paranoia, poor social functioning, and a history of substance abuse . Further research will enable a more accurate prediction of those at greatest risk for developing schizophrenia, and thus to whom early intervention efforts should be directed.
You May Like: Bipolar Binge Eating
Identity Disturbance Is Not Intrinsic To Schizophrenia
I imagine a diagnosis like Schizophrenia might provoke a certain amount of questioning, “Who am I?” Reconciling oneself to any serious mental illness is bound to involve some initial identity confusion. But this falls within the normal range of dissociation. Schizophrenia itself, as I understand it, really has nothing at all to do with identity, though I can guess at the likely source of the confusion: the name itself.
schizo means “to split”phrenia means “mind”
It’s easy to see how schizophrenia and dissociative identity disorder got all tangled up together. A split mind sounds at first like an apt descriptor for multiple personalities. But the mind splitting that the name schizophrenia refers to really has nothing to do with personality, with identity. Instead, it references the fractures in cognitive functioning that are the essence of this thought disorder.
Types Of Dissociative Disorders Associated With Sleep
There are five diagnostic categories of DDs in DSM-IV47 including dissociative identity disorder , dissociative fugue, dissociative amnesia, depersonalization disorder, and dissociative disorder not otherwise specified . Of these, three are considered SRDD: dissociative identity disorder, dissociative fugue, and DD NOS. Most but not all patients with SRDD have both daytime DD episodes as well as previous episodes of SRDD.1,48
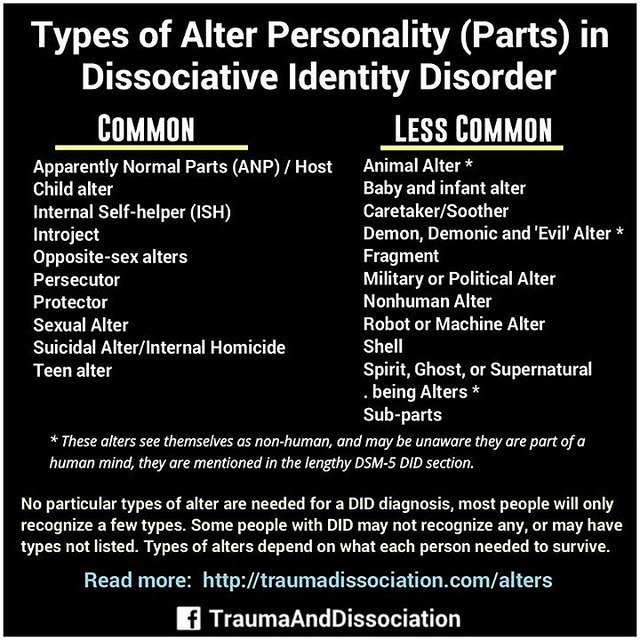
Dissociative Identity Disorder
In dissociative identity disorder, a person displays multiple identities and personalities each with its own pattern of perceiving and integrating with the environment. A minimum of two personalities is required.
Dissociative Fugue State
The dissociative fugue state is characterized by reversible amnesia for personal identity and memories usually lasting hours to days. A dissociative fugue state usually involves unplanned travel or wandering and is sometimes associated with establishment of a new identity. After the episode, prior memories return but there is amnesia for the fugue episode.
Dissociative Disorder Not Otherwise Specified
The classification DD NOS is used for a DD that does not fit the criteria for a specific DD.
Epidemiology
Diagnosis of SRDD
The ICSD-2 diagnostic criteria are listed in Box 2817 and important facts are displayed in Box 2818.
Treatment of SRDDs
E. Cardeña, in, 2017
Also Check: Celine Dion Anorexic
Dissociative Identity Disorder Is Marked By Profound Identity Disturbance
DID was formerly labeled Multiple Personality Disorder for a reason: the disorder is marked by identity disturbance so severe that the sufferer experiences himself not as one person, but many. Rather than the normal levels of identity confusion and identity alteration we all experience, people with Dissociative Identity Disorder live with such profound degrees of both that they appear to have multiple personalities.
In simple terms, what that means is that all the various aspects that make up a person’s identity are separated and walled off from each other in those with Dissociative Identity Disorder. Each aspect of the dissociative identity is real. The disorder isn’t that we’re perceiving the existence of people who don’t actually exist. DID isn’t a thought disorder like Schizophrenia is. It’s a dissociative disorder. In other words, what makes DID a disorder is not these pieces of identity, but how separated those pieces are.
How Is Did Different From Schizophrenia
There are a lot of misconceptions surrounding both DID and schizophrenia. Many people inaccurately believe that people with schizophrenia have split personalities. This isnt the case.
This isnt even technically true of DID. The Sidran Institute says that, although these personalities may feel or appear different, Theyre all manifestations of a single, whole person.
While some symptoms do overlap between DID and schizophrenia, they are different in important ways, including their causes, treatments, and age of onset.
Also Check: Definition Phobia
Myth: Dissociative Identity Disorder Is The Same As Schizophrenia
Fact: Dissociative identity disorder and schizophrenia are not related.
The misconception regarding dissociative identity disorder and schizophrenia is largely caused by focusing on a few key parts of symptoms rather than the disorder as a whole. Dissociative identity disorder refers to a condition in which multiple fully formed personality alters co-exist and shift within one person. Schizophrenia is a psychotic disorder in which a person experiences extreme delusions and hallucinations.
Once A Person Is Being Treated For A Dissociative Disorder How Can Family Members Best Support And Help Him/her
Be open and accepting in your responses. Do not take sides with one or another component of their identity. Rather view them as portions of the person as a whole. We are all different in different situations, but we see this as different sides of ourselves. Try to maintain that perspective with the person with dissociative disorder. Also, help them to protect themselves from any trauma, abuse, or self harm.
Recommended Reading: Schizophrenia Inheritance Rate
Early Warning Signs Of Schizophrenia
In some people, schizophrenia appears suddenly and without warning. But for most, it comes on slowly, with subtle warning signs and a gradual decline in functioning, long before the first severe episode. Often, friends or family members will know early on that something is wrong, without knowing exactly what.
In this early phase of schizophrenia, you may seem eccentric, unmotivated, emotionless, and reclusive to others. You may start to isolate yourself, begin neglecting your appearance, say peculiar things, and show a general indifference to life. You may abandon hobbies and activities, and your performance at work or school can deteriorate.
Risk Factors For Bipolar Disorder And Schizophrenia
No one knows what causes bipolar disorder or schizophrenia. However, genetics are probably a risk factor, as both conditions likely run in families. This doesnt mean that youll definitely inherit the disorder if your parent or sibling has it. Your risk increases, however, if multiple family members have the disorder. But knowing theres a risk increases the chance of early detection and treatment.
Environmental factors may also contribute to your risk, but this connection isnt entirely understood yet.
Recommended Reading: Can Anxiety Raise Blood Sugar
Myth: Violence Is Common Among Individuals With Schizophrenia
Reality: Its actually rare for someone with schizophrenia to be violent, says Dr. Rego. An individual with schizophrenia is much more likely to be the victim of violence rather than the perpetrator, he says. They tend to struggle more to have the social benefits that most of us have, Dr. Rego explains. They may be homeless or staying in a shelter, where they may be singled out and assaulted.
Some individuals with psychiatric disorders like schizophrenia do become aggressive, says Scott Ira Krakower, DO, assistant unit chief of psychiatry at Zucker Hillside Hospital in Glen Oaks, New York. However, it is a myth that this is always the case, he says. A person can be aggressive and have an anger problem and not have schizophrenia, he explains. Both medication and counseling can help with any signs of violent behavior, he says.