Challenges In Diagnosing Schizophrenia
Psychiatric symptoms exist on continua from normal to pathological, meaning the threshold for diagnosis of schizophrenia in clinical practice can be challenging. The clinical diagnosis of schizophrenia relies heavily on the positive symptoms associated with a prolonged psychotic episode. However, a relatively high percentage of the general population report delusional experiences or hallucinations in their lifetime,,, but for most people these are transient. Psychotic symptoms are also not specific to a particular mental disorder. The clinical efficacy of antipsychotic drugs is heavily correlated with their ability to block subcortical dopamine D2 receptors, , suggesting dopamine signalling is important. In spite of this, no consistent relationship between D2 receptors and the pathophysiology of schizophrenia has emerged, . In contrast, the clinical evidence points towards presynaptic dopamine dysfunction as a mediator of psychosis in schizophrenia.
Dopamine Cannabinoids And Schizophrenia
Owing to the historical prominence and wide familiarity of the dopamine hypothesis of schizophrenia, a natural question to ask is whether the psychotomimetic effects of cannabis are mediated by dopamine . Dopamine response is clearly blunted among chronic cannabis users, showing a dose-dependent effect . However, the degree of this effect is not correlated with the level of psychotic symptoms in these users , and the magnitude of the dopamine release also does not correlate with the degree of psychotic symptoms that are acutely produced by cannabinoids . These findings suggest that the effects of cannabis on psychosis are not explained by these alterations in the dopaminergic system. The modern dopaminergic hypothesis of schizophrenia is much more complex than hypothesizing cortical hypofunctioning and mesolimbic hyperfunctioning, and readers wanting a more in-depth analysis of the dopamine hypothesis of schizophrenia are directed to recent reviews on the subject .
Implications For The Dopamine Hypothesis Of Schizophrenia
It is important to distinguish between the dopamine hypothesis of schizophrenia and the dopamine hypothesis of antipsychotic drug action. The latter proposes that reduction of dopaminergic function via either blockade of postsynaptic receptors or attenuation of presynaptic neuronal activity underlays the therapeutic effect of most known antipsychotic agents. Conversely, the former takes this concept a stage further and from it proposes that dopaminergic hyperfunction, via either supersensitivity of postsynaptic receptors or elevated activity of presynaptic neuronal activity, is an important element in the pathophysiology of schizophrenia .
Though it remains important not to overlook the possible role of non-dopaminergic systems in the pathophysiology of schizophrenia and in antipsychotic drug action , it should be emphasized that clarification of whether selective D1 antagonists do or do not show therapeutic efficacy in this disorder will be a watershed in the evolution of these concepts . Furthermore, the putative roles of individual, molecular biologically defined members of the D1-like and of the D2-like families of dopamine receptor in mediating antipsychotic activity remain enigmatic, but may in the future challenge further our present perspectives.
David L. Atkinson, Jeff K. Abbott, in, 2018
Don’t Miss: Does Pristiq Help With Anxiety
Can We Objectively Test Positive Symptom Connectivity In Rodents
Clearly, alternative behavioural phenotypes in animal models, consistent with the underlying neuroanatomical/biological features of schizophrenia, need to be established. This does not invalidate our current rodent models it just emphasises that, in light of the recent compelling PET evidence in patients, we need to review their relevance to the positive symptoms of schizophrenia. Psychosis, an extremely human syndrome, will never be truly observable in rodents. However, we can, and should, aim to establish more translationally relevant tests for the underlying neurobiology of psychosis. Ultimately, we need better behavioural tests for positive symptoms in animal models that will lead to therapies efficacious for both positive and cognitive symptoms in patients. We contend that tests aimed at understanding associative striatal function are imperative. We propose that a combination of cognitive behavioural tasks, that can be tested similarly in humans and rodents , represents our best opportunity to assess positive symptom neurobiology in animal models. It is important to consider that neither task alone is a reliable indicator of positive symptom neurobiology however, in combination they can help isolate associative striatal function.
Fig. 4: Comparisons for cognitive tests in humans and rodents.
Dopamine Hypothesis Of Schizophrenia
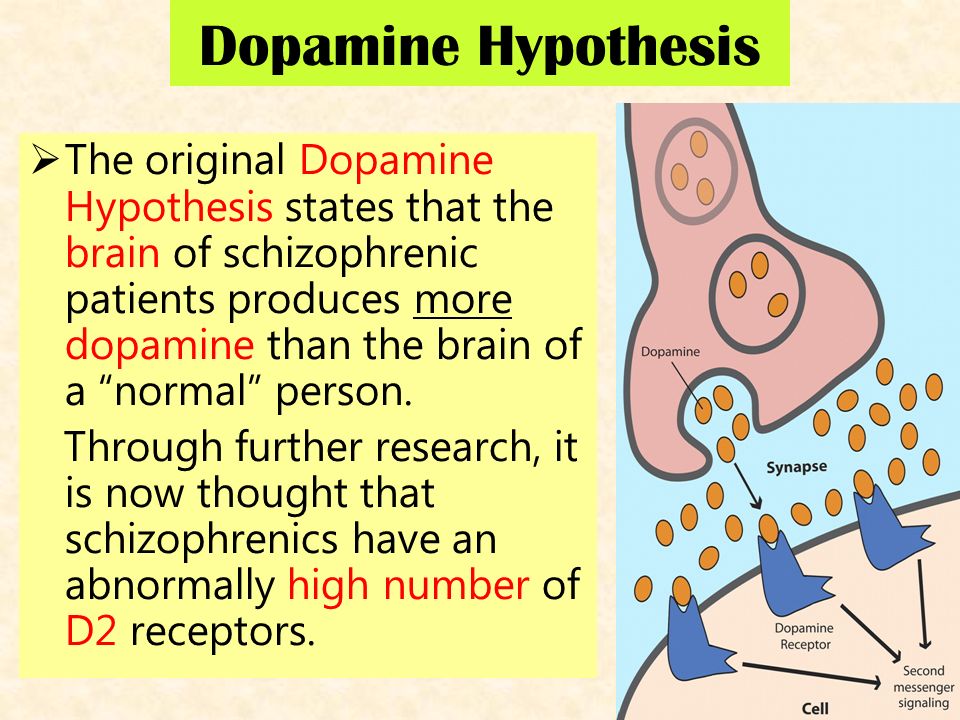
The dopamine hypothesis of schizophrenia or the dopamine hypothesis of psychosis is a model that attributes the positive symptoms of schizophrenia to a disturbed and hyperactive dopaminergicsignal transduction. The model draws evidence from the observation that a large number of antipsychotics have dopamine-receptor antagonistic effects. The theory, however, does not posit dopamine overabundance as a complete explanation for schizophrenia. Rather, the overactivation of D2 receptors, specifically, is one effect of the global chemical synaptic dysregulation observed in this disorder.
Also Check: What Is The Meaning Of Phobia
Elevation Of D2high In Dopamine
The factors that cause behavioural dopamine supersensitivity are listed in Figure 20, all of which influence the proportion of D2High.
Of the many animal models of psychosis that have been proposed, the model of amphetamine sensitization has received much support. Although the amphetamine-sensitized animal is supersensitive to amphetamine, the density of D2 in the brain striatum is normal. The D2High receptors in the striatum, however, were elevated by 250% . Another example, using a different method, is in Figure 22 .
Many types of brain lesions have been proposed as models for schizophrenia, including lesions of the neonatal hippocampus , cholinergic lesions of the cerebral cortex, the entorhinal cortex , and the medial pre-frontal cortex.
Dopamine behavioral supersensitivity also occurs after many types of drug treatment and in mice with specific gene deletions Figure 22 and Figure 23 summarize the enhanced levels of D2High receptors in the brain striata of such gene-deleted mice with behavioral dopamine supersensitivity.
While dopamine supersensitive knockout mice do not reveal elevation in the density of D2, an elevation occurs in D2High in all the brain striata of knockout mice that had previously shown behavioral dopamine supersensitivity.
Deletions of genes that are not related to the dopamine system also yield animal models of behavioral dopamine supersensitivity and at the same time reveal marked elevations in D2High receptors. These genes are listed in Figure 23.
Modelling Psychosis: The Use Of Animal Models
Potentially, the most useful avenue for animal models to assist in schizophrenia research will be identifying convergent aetiological pathways. Understanding which neurotransmitter systems and brain regions are most involved may help to identify the core neurobiological features of schizophrenia. For example, changes in dopaminergic systems are observed in animal models after manipulation of factors based on schizophrenia epidemiology, , genetics, pharmacology and related hypotheses. These include changes in early dopamine specification factors, , sensitivities to psychostimulants,,, and alterations in dopamine neurochemistry,,, . Evidence of subcortical dopaminergic hyperactivity or sensitivity in animal models is proposed to represent the face validity for psychosis in patients. The most commonly used behavioural assessments of positive symptoms in animal models include enhanced amphetamine-induced locomotion and deficits in prepulse inhibition . These tests are widely used because they are relatively simple to perform. However, we propose that given current knowledge of the neurobiology in schizophrenia, they have outlived their usefulness as measures of positive symptoms.
You May Like: Spasmenagaliaphobia
Findings From The Prodrome And Extended Phenotype Of Schizophrenia
A further development since version II of the dopamine hypothesis is the evidence regarding structural differences prior to the onset of schizophrenia. Individuals with prodromal signs also show brain structural deficits, quite like those in patients, although to a lesser degree , as do the relatives of people with schizophrenia and people with schizotypal features . These brain abnormalities are in frontotemporal regionsthe same areas where lesions in animals result in striatal dopaminergic abnormalities.,, There is also evidence of longitudinal brain structural changes in schizophrenia and people at risk of schizophrenia., However, the contribution of factors such as medication, and cannabis use to the longitudinal brain changes has yet to be fully resolvedas such these changes are not addressed in the proposed dopamine hypothesis: version III. It is not just brain structure that is altered in these individuals at risk of schizophreniathere are functional differences as well that are generally in similar brain regions to those seen in schizophrenia and a similar pattern of neurocognitive impairments to those seen in schizophrenia, although again to a lesser degree .
What Are The Symptoms Ofschizophrenia
AmericanPsychiatric AssociationDiagnostic and StatisticalManual of Mental Disorders, Fifth Edition
When people show any of these five symptoms, they are considered to be inthe “active phase” of the disorder. Oftenpeople with schizophrenia have milder symptoms before and after the active phase.
There are three basic types of schizophrenia. All people who haveschizophrenia have lost touch with reality. The three main types ofschizophrenia are:
You May Like: Antidepressant-induced Hypomania
Multiple Routes To Dopamine Dysfunction: Interacting Environmental And Genetic Factors
Genes and environmental factors do not exist in isolation. Many add to each other, and some show synergistic effects on the risk of schizophrenia or brain abnormalities associated with schizophrenia . Furthermore, animal studies indicate that at least some of these factors interact in their effects on the dopamine system: social isolation rearing potentiates the later effects of stimulants, or of stress on the dopamine system. Similar effects have also been found in humans, where striatal dopamine release in response to stress was increased in people who reported low maternal care during their early childhood. Additionally, there are interactions with other neurotransmitter systems: dopamine release is not seen under the influence of ketamine alone but enhances the action of amphetamine, suggesting the effects of NMDA blockade, or by extension other putative causes of glutamatergic dysfunction, such as neonatal insults, are modulatory. GABA interneurons are also involved in the regulation of subcortical dopamine function and have been implicated in schizophrenia.
Challenging Longstanding Assumptions And Moving Forward
Clozapine, discovered in the 1960s, remains the most effective antipsychotic medication, although its use is restricted due to its side effect profile. This stagnation in drug development for schizophrenia highlights a key weakness in schizophrenia research a lack of effective bi-directional translation between basic and clinical research. The fact that the current methods of testing for psychotic symptoms in rodents are now misaligned with recent clinical evidence indicates a need to advance how positive symptoms are examined in animal models. We have proposed a combination of behavioural tests in rodents that are sensitive to dysfunction at the primary site of dopaminergic neurobiology observed in schizophrenia. There will never be a perfect model for psychosis in rodents, but it is critical that we acknowledge the limitations of current methods so that an active dialogue is established.
Recommended Reading: Pristiq For Social Anxiety
What Occurs In The Brain
| The picture below showsmagnetic resonance image brain scans of a pair of twins:one with schizophrenia, one without schizophrenia. Notice that theventricles are larger in the twin withschizophrenia. |
A reduced size of the hippocampus, increased size of the basal ganglia,and abnormalities in the prefrontal cortex are seen in some people withschizophrenia. However, these changes are not seen in all people withschizophrenia and they may occur in people without this disorder.
Alternate Neurochemical Models In Schizophrenia And Their Interactions With Dopamine
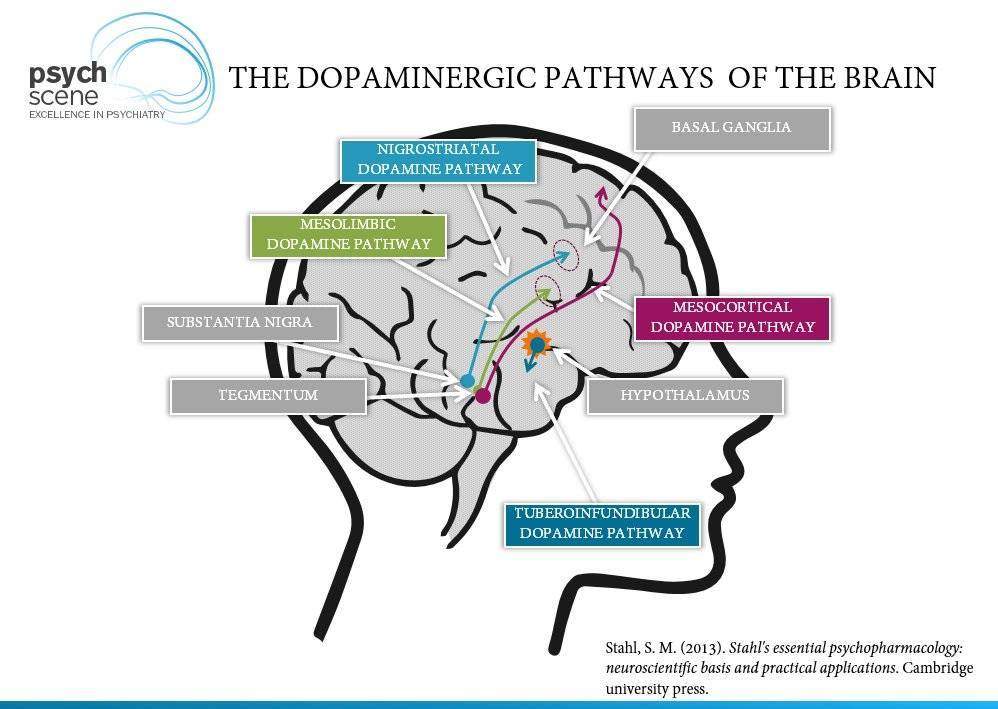
Deviations in dopamine and glutamate have been reported in the prefrontal cortex of schizophrenia patients . NMDA-receptors are involved in releasing dopamine into the striatum and frontal cortex in schizophrenia patients and in rats in an animal model of schizophrenia . These interactions are accompanied by calcium-dependent changes and exchanges between DAT and G72 in various brain regions . In contrast to dopamine receptors, glutamate receptors are found in the subcortical and cortical brain regions . The activity of dopamine is regulated by GABA and glutamate. For example, corticostriatal glutamatergic pathways interact with dopamine terminals , and specific glutamate receptors in the striatum, such as mGlu2, are sensitive to dopamine . High glutamate levels have been found in the dorsal caudate nucleus of schizophrenia patients . Adenosine interacts with glutamate, NMDA-receptors, and dopamine . It can be summarized that NMDA-receptors and D -receptors in cortical brain areas such as the prefrontal cortex and an excess of D -receptors in subcortical brain areas such as the striatum are interconnected with each other through a positive feedback mechanism . However, through its presynaptic action, dopamine reduces the release of glutamate in the pyramidal neurons of layer V in the prefrontal cortex . Dopamine dysregulation in the basal ganglia of schizophrenia patients is an important intrinsic feature in the pathology of schizophrenia and not a medication side effect .
Also Check: What Is The Meaning Of Phobia
Biochemical Factors Controlling The D2high State
The rate of interconversion between the high- and low-affinity states of a G protein-linked receptor may be minutes or seconds. There are many factors that increase the prevalence of the high-affinity state and, therefore, the sensitivity of the tissue to the agonist.
RGS9 co-localizes with D2 in the striatum and accelerates the termination of D2-triggered events. A reduction in RGS9, as occurs in RGS9 knockout mice, leads to behavioral dopamine supersensitivity and a marked increase in the proportions of D2High receptors in the striatum .
The reduced expression of RGS9-2 in schizophrenia hippocampus is consistent with supersensitivity and increased D2High levels.
Because D2High receptors are consistently elevated in all the animal models of the various human psychoses, and because the majority of psychotic episodes respond to D2 blockade, D2High may be a common target for the convergence of the various psychosis pathways. Consistent with this hypothesis of D2High is the fact that most psychoses respond to treatment with D2 antagonists, including phencyclidine psychosis . The treatment of phencyclidine psychosis by haloperidol is significant, because haloperidol does not block NMDA receptors, indicating that the D2 target is critically active in phencyclidine psychosis .
The negative aspects of psychosis, especially cognition, which is impaired in schizophrenia, may arise from overexpression of D2 in the striatum .
Support From Genetic Studies
Genetic evidence has suggested that there may be genes, or specific variants of genes, that code for mechanisms involved in dopamine function, which may be more prevalent in people experiencing psychosis or diagnosed with schizophrenia. Dopamine related genes linked to psychosis in this way included COMT and DRD4.
- Main article: Schizophrenia – Genetic factors
Recommended Reading: How To Cure Schizophrenia Permanently
What Is The Dopamine Hypothesis Of Schizophrenia
The dopaminehypothesis of schizophrenia is a theory about how people develop that mental illness. Dopamine is an important neurotransmitter in the brain that moderates basic behaviors like motivation. This hypothesis argues that overproduction or excessive release of dopamine is part of what causes schizophrenia. Evidence from brain imaging and pharmacology supporting the hypothesis includes the observation that drugs that cause psychosis also cause increased activity in neural pathways that depend on dopamine. Scientists do not agree on whether the dopamine hypothesis is correct.
Animal Models Of Psychosis
Many animal models for psychosis and schizophrenia have been proposed. The majority of these models show behavioural dopamine supersensitivity and an elevation of D2High.
Various brain injuries or treatments related or unrelated to dopamine can result in dopamine supersensitivity, the latter being an aspect of schizophrenia, as already noted.
Considering the many interconnecting pathways in the brain, it is not surprising that various types of injury to the brain by drugs, brain lesions, or by gene mutations in specific neurotransmitter pathways can result in major biochemical alterations in another completely different pathway.
Recommended Reading: Is Sex Good For Depression
Environmental Risk Factors For Schizophrenia
A large number of disparate environmental factors clearly contribute to the risk for schizophrenia, yet many hypotheses of schizophrenia, including previous versions of the dopamine hypothesis, make no allowance for them. Markers of social adversity such as migration, unemployment, urban upbringing, lack of close friends, and childhood abuse are all associated with a well-established increased risk for schizophrenia that cannot readily be explained by genetic factors alone. These factors either directly index social isolation/subordination or are linked to these experiences. Studies in animals of social isolations and subordination, find that these factors lead to dopaminergic overactivity.
Which Of The Three D2
The D3 receptor has been extensively investigated for linkage and association to schizophrenia , but the results remain controversial. The only D3-selective drug that has been tested against schizophrenia is BP897 at 10 mg per day for 4 weeks, a dose that did not attain a significant antipsychotic effect.
Likewise, the D4 receptor, although earlier thought to be elevated in schizophrenia, has not been found to be a main target for schizophrenia treatment.
An example of D2 occupancy is given in Figure 15, where the % of D2 receptors occupied by risperidone is approximately 70% at the average therapeutic daily dose of 2 to 6 mg. The data in Figure 14 and Figure 15 are consistent with the point of Figure 1 that the main target for antipsychotic action is the D2 receptor.
Recommended Reading: Does Donald Duck Have Ptsd
Treatment And Dopamine Receptors
Over 120 neurochemical imaging studies have investigated the in vivo effects of antipsychotic treatments on dopamine receptors in schizophrenia . These show that at clinical doses all currently licensed antipsychotic drugs block striatal D2 receptors. Furthermore, a threshold striatal D2 blockade is required for antipsychotic efficacy, but this is not sufficientsome patients show little improvement despite high D2 occupancy. A major stumbling block for the dopamine hypothesis used to be the notion that antipsychotic response was delayed for 23 weeks after the start of treatment . However, there is now convincing evidence that there is no delayed response: the onset of antipsychotic action is early,, this response is related to striatal D2 receptor occupancy, and D2 occupancy at as early as 48 hours predicts the nature of response that follows over the next 2 weeks. Thus, the original tenet of version I still standsdopamine D2 receptors continue to dominate and remain necessary for antipsychotic treatment and the imaging data has further strengthened the quantitative and temporal aspects of this relationship.