Box : Symptom Groups In Schizophrenia
-
Positive symptoms
: Positive symptoms include delusions and hallucinations, linked to aberrant salience. These symptoms are most recognisable during periods of acute psychosis.
-
Cognitive symptoms
: Impairments in learning, memory, attention and executive functioning are all included as cognitive symptoms.
-
Negative symptoms: Negative symptoms include blunting of affect , avolition and social withdrawal.
It is widely acknowledged that we cannot recreate the complicated symptom profile of schizophrenia in animal models. However, animal models provide an avenue to invasively explore the role of neurotransmitters and circuitry in psychiatric diseases. To improve the poor predictive validity of treatments in animal models, it is critical that our understanding and the use of animal models evolves alongside our knowledge of schizophrenia neurobiology. The delayed incorporation of new clinical findings to develop better animal models highlights the need for better communication between clinical and basic research communities.
In this article, we discuss the challenges clinicians and researchers are facing in understanding the neurobiology of positive symptoms and psychosis in schizophrenia. We discuss the implications this has for current assessments of positive symptoms in rodents and propose a more relevant set of tests for future study. Finally, the need for a joint focus on bi-directional translation between clinical and basic research is outlined.
What Is The Biochemical Basis Of Depression
Steven Gans, MD is board-certified in psychiatry and is an active supervisor, teacher, and mentor at Massachusetts General Hospital.
There are several theories about what causes depression. The condition most likely results from a complex interplay of individual factors, but one of the most widely accepted explanations cites abnormal brain chemistry.
Sometimes, people with depression relate the condition back to a specific factor, such as a traumatic event in their life. However, it’s not uncommon for people who are depressed to be confused about the cause. They may even feel as though they don’t have “a reason” to be depressed.
In these cases, learning about the theories of what causes depression can be helpful. Here’s an overview of what is known about how chemical imbalances in the brain may influence depression.
Examples Of Important Neurotransmitter Actions
As explained above, the only direct action of a neurotransmitter is to activate a receptor. Therefore, the effects of a neurotransmitter system depend on the connections of the neurons that use the transmitter, and the chemical properties of the receptors that the transmitter binds to.
Here are a few examples of important neurotransmitter actions:
Don’t Miss: Does Pristiq Help With Anxiety
Integrating The Dopamine And Glutamate Hypotheses
Whilst the evidence for the involvement of presynaptic dopamine dysfunction in the majority of cases of schizophrenia is compelling, dopamine dysfunction is most clearly linked to psychotic symptoms and the evidence for dopamines involvement in the negative and cognitive symptoms is much less clear-cut . In this respect glutamate models involving NMDA receptor blockade appear to be better able account for the range and nature of these aspects of schizophrenia . A combination of both NMDA hypofunction and presynaptic dopamine dysfunction may therefore provide the best explanation of all the clinical aspects of schizophrenia.
Interactions between glutamatergic and dopaminergic pathways
Whilst the studies discussed above provide evidence that dopamine dysregulation in schizophrenia could be secondary to glutamatergic dysfunction, they do not identify the specific brain circuits or regions involved. The prefrontal cortex and hippocampus have both been suggested as potential sites as both regulate midbrain dopamine neurons via glutamatergic projections to the midbrain .
Hippocampus
Prefrontal cortex
Whilst there are data linking altered frontal function to striatal presynaptic dopamine dysfunction in patients and at risk subjects , we are not aware of any studies investigating the relationship between frontal glutamate to striatal dopamine dysfunction in patients.
The Nmda Receptor Hypofunction Hypothesis
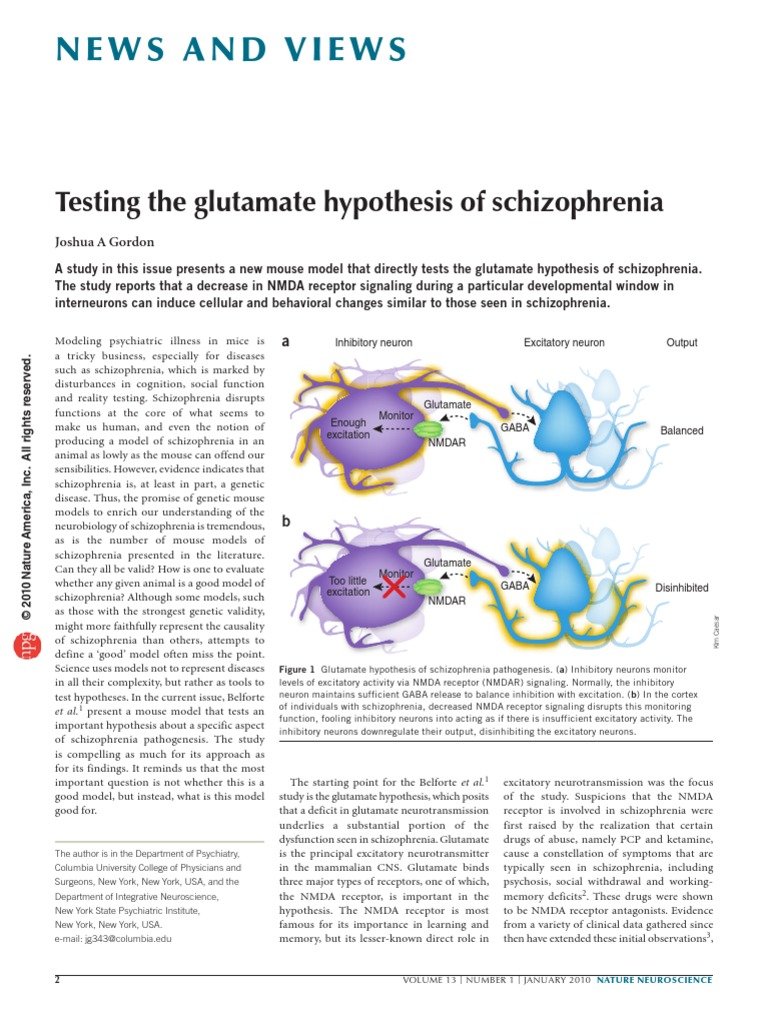
Excitatory neurotransmission in the brain is primarily glutamatergic, with glutamatergic neurons utilising between 60 and 80 percent of total brain metabolic activity . Glutamatergic neurotransmission occurs through metabotropic and ionotropic glutamate receptors, which are each subdivided into 3 groups. Group I metabotropic glutamate receptors are mainly postsynaptic, whereas group II and III are primarily presynaptic and modulate neurotransmitter release . Ionotropic glutamate receptors are named after the agonists originally found to selectively activate them: a-amino-3-hydroxy-5-methyl-4-isoazolepropionic acid , kainate and N-methyl- D-aspartate .
Also Check: What Are The Three Stages Of Schizophrenia
The Role Of Key Neurotransmitters
The three neurotransmitters implicated in depression are:
There are other neurotransmitters that can send messages in the brain, including glutamate, GABA, and acetylcholine. Researchers are still learning about the role these brain chemicals play in depression and other conditions, such as Alzheimer’s and fibromyalgia.
Sleep And Schizophrenia Are Intimately Linked
Since sleep regulation involves many neurotransmitter systems and brain circuits, it is likely that the mechanisms generating normal sleep overlap with those that maintain mental health. This would explain why disturbed sleep and schizophrenia are so intimately linked. This was the essence of the seminar given at the Lundbeck Institute on 17th April 2015 by Russell Foster, director of the Sleep and Circadian Neuroscience Unit at the University of Oxford, UK.
Sleep disturbance is common in serious mental illness, and schizophrenia is no exception. It is widely accepted that schizophrenia disrupts sleep and circadian rhythms. But it also seems that disturbances of sleep can precede severe mental illness and may even help cause it.1
Recommended Reading: Does Pristiq Help With Anxiety
Alternate Neurochemical Models In Schizophrenia And Their Interactions With Dopamine
Deviations in dopamine and glutamate have been reported in the prefrontal cortex of schizophrenia patients . NMDA-receptors are involved in releasing dopamine into the striatum and frontal cortex in schizophrenia patients and in rats in an animal model of schizophrenia . These interactions are accompanied by calcium-dependent changes and exchanges between DAT and G72 in various brain regions . In contrast to dopamine receptors, glutamate receptors are found in the subcortical and cortical brain regions . The activity of dopamine is regulated by GABA and glutamate. For example, corticostriatal glutamatergic pathways interact with dopamine terminals , and specific glutamate receptors in the striatum, such as mGlu2, are sensitive to dopamine . High glutamate levels have been found in the dorsal caudate nucleus of schizophrenia patients . Adenosine interacts with glutamate, NMDA-receptors, and dopamine . It can be summarized that NMDA-receptors and D -receptors in cortical brain areas such as the prefrontal cortex and an excess of D -receptors in subcortical brain areas such as the striatum are interconnected with each other through a positive feedback mechanism . However, through its presynaptic action, dopamine reduces the release of glutamate in the pyramidal neurons of layer V in the prefrontal cortex . Dopamine dysregulation in the basal ganglia of schizophrenia patients is an important intrinsic feature in the pathology of schizophrenia and not a medication side effect .
Brain Chemicals And Depression
Researchers have suggested that for some people, having too little of certain substances in the brain could contribute to depression. Restoring the balance of brain chemicals could help alleviate symptomswhich is where the different classes of antidepressant medications may come in.
Even with the help of medications that balance specific neurotransmitters in the brain, depression is a highly complex condition to treat. What proves to be an effective treatment for one person with depression may not work for someone else. Even something that has worked well for someone in the past may become less effective over time, or even stop working, for reasons researchers are still trying to understand.
Researchers continue to try to understand the mechanisms of depression, including brain chemicals, in hopes of finding explanations for these complexities and developing more effective treatments. Depression is a multi-faceted condition, but having an awareness of brain chemistry can be useful for medical and mental health professionals, researchers, and many people who have depression.
Depression Discussion Guide
Also Check: Does Pristiq Help With Anxiety
What Happens To The Body And Brain Of Individuals With Schizophrenia
Richard C. Deth, a professor of Pharmaceutical Science at Northeastern University, provides this answer:
Schizophrenia is a psychiatric disorder in which previously normal cognitive abilities and behaviors becomes disturbed. The most common age of onset is just after reaching adulthood, typically the late-teens to the mid-thirties. It is manifested either by so-called positive symptoms or by negative symptoms, including a marked lack of activity, loss of interest and unresponsiveness.
Although the precise cause of schizophrenia remains unknown, an enormous amount of research has come up with a number of possibilities. Many early theories focused on behavioral or stress-induced events, but more recently, consensus holds that underlying biochemical abnormalities are more likely the cause. Lending great support to this idea is the fact that genetic predisposition may account for 50 percent of the risk of developing schizophrenia. Not surprisingly, these biochemical hypotheses center on dysfunction of the neurotransmitter systems in the brain, which provide for normal cognition and attention. The main theories include the Dopamine Hypothesis, the NMDA Receptor Hypothesis, the Single-carbon Hypothesis and the Membrane Hypothesis. And new research from our laboratory suggests that elements from each of these theories may play a role in schizophrenia.
Indirect Evidence For Dopamine Dysfunction In Schizophrenia
Animal models
Rodent models of schizophrenia are useful for investigating molecular mechanisms that may be of pathophysiological relevance, and for testing novel therapeutic interventions.
One well characterized model of dopaminergic hyperactivity involves administering repeated doses of amphetamine. This has been shown to induce events that are also observed in individuals with schizophrenia, such as reduced prepulse inhibition, stereotyped behaviours, and impaired cognitive flexibility and attention. Given that amphetamine results in dopamine release, and that the above effects can be ameliorated with the administration of dopamine antagonists, this provides indirect evidence for a role of dopamine in behaviour thought to be a proxy for psychotic symptoms.
Another example is that of mice genetically modified to overexpress dopamine D2 receptors in the striatum, which also display a wide range of schizophrenia-like behaviours. Similarly, transgenic insertion of tyrosine hydroxylase and guanosine triphosphate cyclohydrase 1 into the substantia nigra in early adolescence increases dopamine synthesis capacity, and has been associated with a schizophrenia-like behavioural phenotype.
In summary, multiple methods have been used to induce increased striatal dopamine signalling in animal models, and these consistently produce behaviours analogous to those observed in individuals with schizophrenia.
Cerebrospinal fluid and post-mortem studies
Summary of indirect findings
Don’t Miss: Mayo Clinic Anxiety And Depression
What Neurotransmitters Are Involved In Schizophrenia
DOPAMINE
Two brain chemicals may interact to contribute to the development of psychotic disorders such as schizophrenia, according to a new study. The results suggest abnormal levels of the neurotransmitter glutamate may lead to changes in the levels of another neurotransmitter, dopamine, causing the transition into psychosis.
Beside above, what is the chemical imbalance in schizophrenia? Chemistry: Scientists believe that people with schizophrenia have an imbalance of the brain chemicals or neurotransmitters: dopamine, glutamate and serotonin. These neurotransmitters allow nerve cells in the brain to send messages to each other.
In respect to this, what is the role of dopamine in schizophrenia?
Dopamine gets a lot of attention in brain research because it’s been linked to addiction. It also plays a role in other psychiatric and movement disorders, like Parkinson’s disease. In schizophrenia, dopamine is tied to hallucinations and delusions.
What does serotonin do in schizophrenia?
Moreover, serotonin has been implicated in a variety of behaviors and somatic functions that are disturbed in schizophrenia .
Indirect Evidence For Glutamates Involvement
Post mortem and genetic studies
Post mortem studies provide evidence for alterations to glutamatergic functioning in schizophrenia. Studies of NMDA receptor expression in post mortem samples have produced some positive findings such as reduced NMDAR1 subunit density in the superior frontal cortex and the superior temporal cortex . However, overall findings regarding NMDA receptor density have been inconsistent . It seems that the abnormality in schizophrenia may primarily be aberrant glutamate receptor localisation as opposed to a generalised deficit . This abnormality could arise as a result of changes in glutamate receptor trafficking molecules . Furthermore there is evidence for a variety of functional changes affecting the intracellular effects of the NMDA receptor that would have a major impact on glutamatergic signalling.
The potential role of glutamate in the pathophysiology of schizophrenia is also supported by recent genetics findings . GRIN2A which codes for an NMDA receptor subunit was found to be associated with schizophrenia, as was SRR which plays a key role in pathways leading to the activation of the NMDA receptor.
NMDA receptor antagonists
Glutamatergic drugs treatments for schizophrenia
Read Also: Prodromal Symptoms Of Schizophrenia Are Evident
Other Neurotransmitters In Schizophrenia
Clozapine, which is the most effective medication available for treating the symptoms of Schizophrenia, is a very weak blocker of the D2 dopamine receptors. This suggests that there must be other neurotransmitter systems that are also involved in causing Schizophrenia, though so far not much is known about what are these other factors.
One neurotransmitter that has gotten increased attention in recent years for its role in Schizophrenia in glutamate, which targets NMDA receptors in the brain. Phencyclidine and Ketamine are two drugs that block the actions of glutamate at the NMDA receptor, and these drugs can cause both the positive and negative symptoms of Schizophrenia in people who do not have the condition. Increasing the actions of glutamate by using high doses of precursor molecules that are metabolized into glutamate, such as D-serine, glycine and D-cycloserine, show promise in helping to improve the negative symptoms of Schizophrenia.
Limitations Of The Glutamate Evidence In Schizophrenia
Although several lines of evidence point to there being glutamatergic abnormalities in schizophrenia, there are a number of potential limitations to the theory. The use of 1H-MRS as the primary tool for the in vivo imaging of the glutamatergic system has some limitations. In particular 1H-MRS may not be able to distinguish between intra and extracellular compartments so changes could reflect alterations in either compartment. The development of specific radiotracers for imaging of NMDA and AMPA receptors will potentially enable the extracellular release of glutamate to be studied. 13C MRS is another potentially useful tool for allowing clearer understanding of the glutamatergic system. A further limitation of the glutamate hypothesis is that it is not clear exactly what NMDA hypofunction means at the molecular level. This partly reflects the limitations of the evidence available at the moment.
Don’t Miss: What Are The Three Stages Of Schizophrenia
Current Issues And Challenge
The history of the search for genes contributing liability to schizophrenia is around a quarter of century old, but it is always dashed with nonreplication of the finding. This has been so despite consistent evidence from family, twin and adoption studies of an important genetic contribution the heritability of schizophrenia is estimated to be approximately 80% . The reasons for the difficulty in finding genes include the complexity of the phenotype, heterogeneity and lack of biological marker. The mode of transmission is multifactorial where non-genetic determinants are also operating. As has been pointed earlier, schizophrenia does not conform to a classical Mendelian pattern of inheritance and it is now clear that most, perhaps all, cases involve the combined effects of many genes, each conferring a small increase in liability to the disorder not due to single gene of major effects. As a consequence, a single gene does not seem to cause the disorder thus no causal disease genes, only susceptibility genes are operating. Otherwise a consistently replicable linkage signal should have been detected. Advancement has also been hampered by the relatively small size of many studies. Not only are large sample needed to detect small effects, but even larger samples are needed to replicate positive findings
An Overview Of Neurotransmitters And Mental Health During Brain Awareness Week
Brain Awareness Week is March 12-18. The annual event focuses attention on the importance of the brain and the work of partner organizations around the world. Activities run the gamut from exhibitions about the brain to brain-themed lectures to open house events at neuroscience labs. There are also special displays at libraries and community gathering places, classroom workshops and other events. The goal is to engage people of all ages and provide information on this most important of organs and one we too often take for granted. Its also an excellent time for providers of mental health services to share insights on how the workings of the brain affect mental health.
You May Like: How To Help People With Depression
Sleep Draws Upon All Of The Neurotransmitter Systems Of The Brain
Sleep draws upon all of the neurotransmitter systems of the brain
If these ideas can be substantiated, sleep would represent a new therapeutic target, both in the prevention of mental illness and its treatment. And there is evidence from a pilot study that cognitive behaviour therapy for insomnia can improve the condition of schizophrenic patients with persistent persecutory delusions.5 This study evaluated the treatment of insomnia in individuals with persecutory delusions to establish whether reducing insomnia will reduce paranoid delusions. In 15 patients who received cognitive behavioural intervention for insomnia intervention, levels of insomnia and persecutory delusions were significantly reduced post-treatment and at one-month follow-up. Levels of anomalies of experience, anxiety and depression were also reduced. It was concluded that CBT-I can be used to treat insomnia in individuals with persecutory delusions and also lessens the delusions.
More broadly, we should aim to develop strategies that can help patients with schizophrenia consolidate sleep and so help improve their quality of life.
Dopaminergic Features Of Psychosis In Schizophrenia
In healthy individuals, dopamine stimulants such as amphetamine can induce psychotic symptoms, and people with schizophrenia are more sensitive to these effects, . Studies using positron emission tomography imaging have shown patients with schizophrenia show increases in subcortical synaptic dopamine content, , abnormally high dopamine release after amphetamine treatment,,,,, and increased basal dopamine synthesis capacity ,, compared with healthy controls. Increased subcortical dopamine synthesis and release capacity are strongly associated with positive symptoms in patients, , and increased subcortical synaptic dopamine content is predictive of a positive treatment response. It was widely anticipated that the limbic striatum would be confirmed as the subdivision where these alterations in dopamine function would be localised in patients. The basis for this prediction was the belief that reward systems were aberrant in schizophrenia. However, as PET imaging resolution improved it was found that increases in synaptic dopamine content, and synthesis capacity were localised, or more pronounced, in the associative striatum . Furthermore, alterations in dopamine function within the associative striatum likely contribute to the misappropriate attribution of salience to certain stimuli, a key aspect of delusions and psychosis.
Also Check: Phobia Of Bees