The Cabrera Display For Diagnosing Acute Coronary Syndrome
The ECG is an essential diagnostic tool, since it is available very early in the management of patients with suspected acute coronary syndrome, often considerably earlier than biomarkers and other diagnostic modalities. The electrocardiographic diagnosis of ST-elevation myocardial infarction is based on presence of significant ST elevation in at least 2 anatomically contiguous leads . In the standard presentation anatomically contiguous leads are not presented adjacently, which makes it unnecessarily difficult for the inexperienced ECG reader to apply the STEMI criteria. Only 3 lead pairs in the frontal plane can easily be recognized aVL/I, II/aVF and III/aVF. In the Cabrera format, 2 additional lead pairs are evident I/aVR andaVR/II.
Electrocardiogram Standard Limb Leads
Bipolar recordings utilize standard limb lead configurations depicted in the figure. By convention, lead I has the positive electrode on the left arm, and the negative electrode on the right arm, and therefore measures the potential difference between the two arms. In this and the other two limb leads, an electrode on the right leg serves as a reference electrode for recording purposes. In the lead II configuration, the positive electrode is on the left leg and the negative electrode is on the right arm. Lead III has the positive electrode on the left leg and the negative electrode on the left arm. These three bipolar limb leads roughly form an equilateral triangle that is called Einthoven’s triangle in honor of Willem Einthoven who developed the electrocardiogram in the early 1900s. Whether the limb leads are attached to the end of the limb or at the origin of the limb makes little difference in the recording because the limb can simply be viewed as a long wire conductor originating from a point on the trunk of the body.
For a heart with a normal ECG and a mean electrical axis of +60°, the standard limb leads will appear as follows:
See also:
Right Ventricular Ischemia/infarction: Ecg Leads V3r V4r V5r And V6r
Infarction of the right ventricle is unusual but may occur if the right coronary artery is occluded proximally. None of the standard leads in the 12-lead ECG is adequate for diagnosing right ventricular infarction. However, V1 and V2 may occasionally display ECG changes indicative of ischemia located in the right ventricle. In such scenarios, it is recommended that additional leads be placed on the right side of the chest. These leads are V3R, V4R, V5R and V6R, which are placed on the same anatomical locations as their left sided counterparts. Refer to Figure 22.
You May Like: Blurred Vision Panic Attack
Ecg Leads: From Electrodes To Limb Leads Chest Leads & 12
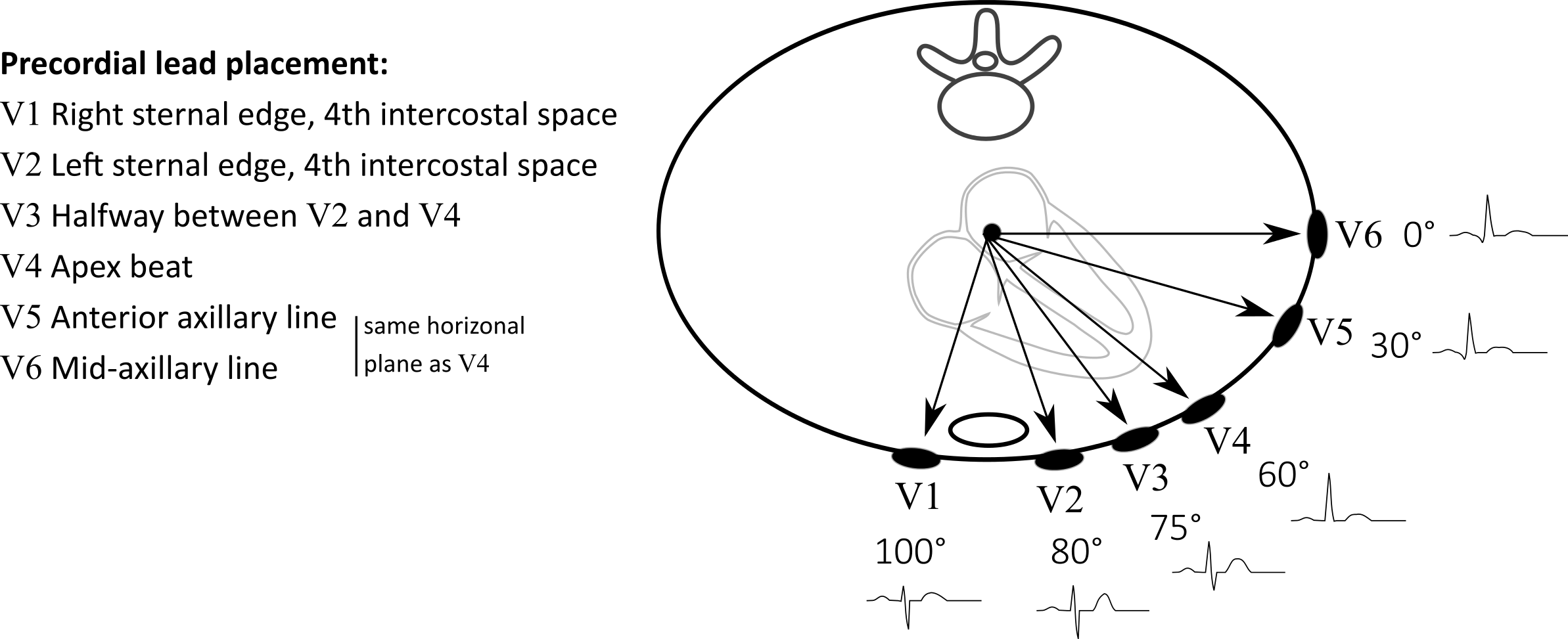
Before discussing the ECG leads and various lead systems, we need to clarify the difference between ECG leads and ECG electrodes. An electrode is a conductive pad that is attached to the skin and enables recording of electrical currents. An ECG lead is a graphical description of the electrical activity of the heart and it is created by analysing several electrodes. In other words, each ECG lead is computed by analysing the electrical currents detected by several electrodes. The standard ECG which is referred to as a 12-lead ECG since it includes 12 leads is obtained using 10 electrodes. These 12 leads consists of two sets of ECG leads: limb leads and chest leads. The chest leads may also be referred to as precordial leads. This article will discuss the ECG leads in detail and no prior knowledge is required. Note that the terms unipolar leads and bipolar leads are not recommended because all ECG leads are bipolar, since they compare electrical currents in two measurement points.
Calculation Of Ecg Parameters
As this study aimed to examine the temporal evolution of AF organization indices in a way that would be clinically applicable, several different factors were considered when choosing appropriate analysis methods, including the non-stationary and multi-variate nature of ECG signals recorded in AF, as well as the feasibility of a real-time implementation. Various time-frequency approaches exist for estimating frequency in non-stationary data. The cross Wigner-Ville distribution was for example used in Stridh et al. to estimate the IF on the single ECG leads V1, V2, and V3. However, these methods can only estimate frequency instantaneously insofar as their time-frequency resolution compromise allows. Additionally, these methods are not designed for multivariate applications, and so do not inherently take advantage of the redundancy that exists between signals recorded on each of the six precordial ECG leads, which can be exploited to provide better overall performance and robustness . Empirical mode decomposition for time-frequency analysis has been extended for multi-variate applications, and has found data-adaptive application in tracking variations in the characteristic 10-Hz rhythm found in EEG signals . However, this method requires that signals be available in their entirety and so would not be suitable for a real-time application.
2.4.1. Adaptive Frequency Tracking
2.4.2. ECG-Based Organization Indices
You May Like: What Is The Phobia Of Throwing Up Called
Who Should Have A 12
The main purpose of the 12-lead ECG is to screen patients for possible cardiac ischemia. It helps EMS and hospital staff to quickly identify patients who have STEMI and perform appropriate medical intervention based on initial readings.
To measure the hearts electrical activity accurately, proper electrode placement is crucial.
In a 12-lead ECG, there are 12 leads calculated using 10 electrodes.
Ecg Parameters Before And During Ablation
Figure 3. IF at pre-PVI, dur-PVI, and post-PVI for all patient groups. Significant differences between groups at each ablation step are displayed **p< 0.01.
Figure 4. AOI calculated on leads V1, V3, V4, and V6b at pre-PVI, dur-PVI, and post-PVI for all patient groups. Significant differences between groups at each ablation step are displayed *p< 0.05, **p< 0.01. Leads V2 and V5 not shown, as results were not significant on these leads.
Also Check: Schizophrenia Inheritance Rate
Temporal Evolution Of Af Organization Post
Atrial fibrillatory waves were not consistently observed in the post-PVI ECG signals of three patients. Since this precluded reliable atrial activity extraction for a sufficient number of epochs, the data from these patients were excluded from this part of the analysis. Additionally, two LTN patients reached the procedural endpoint dur-PVI therefore, post-PVI analysis was not feasible. Figures 6, 7 show examples of the three types of AF organization outlined in section 2.7 for IF, AOI, SampEn, and FWA .
Figure 6. Three types of AF organization. The observed relative percent change is indicated in the title of each example. The first column shows examples of Type 1, increasing AF organization, indicated by a negative IF transition in the first row and a positive AOI transition in the second row. The second column shows examples of Type 2, decreasing AF organization, indicated by a positive transition in the IF epoch sequence, and negative transition in the AOI epoch sequence. Finally, the third column shows examples of Type 3, no change in AF organization, indicated by no transitions in either sequence.
Table 2. Relative changes in IF and AOI post-PVI, according to ablation outcomes, expressed as median with percentiles.
Table 3. Relative changes in SampEn and FWA post-PVI, according to ablation outcomes, expressed as median with percentiles.
Table 4. Relative changes in IF and AOI post-PVI, according to form of recurrence, expressed as median with percentiles.
Alternative Ecg Lead Systems
The conventional placement of electrodes can be suboptimal in some situations. Electrodes placed distally on the limbs will record too much muscle disturbance during exercise stress testing electrodes on the chest wall may be inappropriate in case of resuscitation and echocardiographic examination etc. Efforts have been made to find alternative electrode placements, as well as reducing the number of electrodes without loosing information. In general, lead systems with less than 10 electrodes can still be used to compute the all standard leads in the 12-lead ECG. Such calculated ECG waveforms are very similar to the original 12-lead ECG waveforms, with some minor differences that may affect amplitudes and intervals.
As a rule of thumb, modified lead systems are fully capable of diagnosing arrhythmias but one should be cautious when using these systems to diagnose morphological conditions that dependent on criteria for amplitudes and intervals . Indeed, in the setting of myocardial ischemia one millimeter may make a life-threatening difference.
Lead systems with reduced electrodes are still used daily to detect episodes of ischemia in hospitalized patients. This is explained by the fact that when monitoring continuously i.e when assessing ECG changes over time the initial ECG recording is of minor importance. Instead the interest lies in the dynamics of the ECG and in that scenario the initial recording is of little interest.
Read Also: Definition Of Phobic
Ecg Lead Avr Avf And Avl
These leads were originally constructed by Goldberger. In these leads the exploring electrode is compared with a reference which is based on an average of the other two limb electrodes. The letter a stands for V for voltage and R is right arm, L is left arm and F is foot.
In aVR the right arm is the exploring electrode and the reference is composed by averaging the left arm and left leg. Lead aVR can be inverted into lead aVR , which is identical to aVR but upside-down. There are three advantages of inverting aVR into aVR:
Despite these advantages lead aVR is unfortunately still used in the United States and many other countries. Luckily, all modern ECG machines can be configured to show either aVR or aVR. We recommend the use of aVR but for the purpose of this course we will frequently present both leads. If only one of these leads is shown, the reader may simply turn it upside-down to get a view of the desired lead. Finally, it should be noted that very few ECG diagnoses depend on lead aVR/aVR.
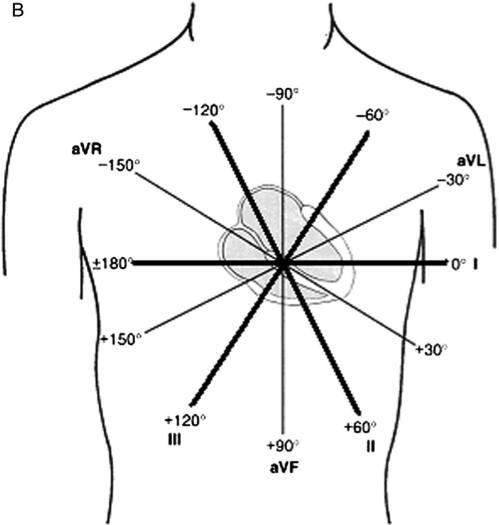
In lead aVL the left arm electrode is exploring and the lead views the heart from 30°. In lead aVF the exploring electrode is placed on the left leg, so this lead observes the heart directly from south.
If And Aoi Temporal Evolution During Step
To investigate the temporal evolution of the IF and AOI during ablation, we calculated the IF and AOI signals for all epochs in the dur-PVI and post-PVI steps. For each patient, we then created a temporal sequence of the mean values of each of the epoch IF and AOI signals, rather than averaging epoch means together, as was done in section 2.5. Therefore, two time sequences, composed of the mean values of the IF and AOI signals found for each epoch, were available for each patient. To test for the presence of a possible transition in the mean of the sequences, we used a statistical approach based on the principle of Minimum Description Length . We compared the MDL values obtained when two different models were used to model the sequence: a model with two parameters , and a model with three parameters . To estimate the second model, all sample indices, except the first and last, were tested as candidates for the index of the transition, with the two means computed using respectively the samples preceding and following the candidate index. The index corresponding to the smallest residual variance was then retained as the transition index. The MDL was computed using
Figure 2. Illustrative example of MDL test. Sequence of random values in which the MDL test found no transition. Sequence of random values, plus step function, in which the MDL test found a transition at the step index, with x the mean value before the transition and y the mean value after the transition.
Also Check: Definition Of A Phobia
Conditions For Which Determination Of The Axis Is Helpful In Diagnosis
-
Conduction defectsfor example, left anterior hemiblock
-
Ventricular enlargementfor example, right ventricular hypertrophy
-
Broad complex tachycardiafor example, bizarre axis suggestive of ventricular origin
-
Congenital heart diseasefor example, atrial septal defects
-
Pre-excited conductionfor example, Wolff-Parkinson-White syndrome
-
Pulmonary embolus
Several methods can be used to calculate the cardiac axis, though occasionally it can prove extremely difficult to determine. The simplest method is by inspection of leads I, II, and III.
Heart Disease And Mental Health Disorders
Mental health is an important part of overall health and refers to a persons emotional, psychological, and social well-being. Mental health involves how we think, feel, act, and make choices.
Mental health disorders can be short- or long-term and can interfere with a persons mood, behavior, thinking, and ability to relate to others. Various studies have shown the impact of trauma, depression, anxiety, and stress on the body, including stress on the heart.1-3
Recommended Reading: Bipolar And Childhood Trauma
What Mental Health Disorders Are Related To Heart Disease
Some of the most commonly studied mental health disorders associated with heart disease or related risk factors include the following:*
Mood Disorders: People living with mood disorders, such as major depression or bipolar disorder, find that their mood affects both psychological and mental well-being nearly every day for most of the day.
Anxiety Disorders: People respond to certain objects or situations with fear, dread, or terror. Anxiety disorders include generalized anxiety, social anxiety, panic disorders, and phobias.
Post-Traumatic Stress Disorder : People can experience PTSD after undergoing a traumatic life experience, such as war, natural disaster, or any other serious incident.
Chronic Stress: People are in a state of uncomfortable emotional stressaccompanied by predictable biochemical, physiological, and behavioral changesthat is constant and persists over an extended period of time.
*There may be other behavioral health disorders, such as substance use disorders, that are connected to heart disease.
What Groups Have Higher Rates Of Heart Disease From Mental Health Disorders
Specific populations, such as the following, show higher rates of heart disease as a result of pre-existing mental health disorders:
Veterans. Studies found that veterans are at a higher risk for heart disease, mainly due to PTSD as a result of combat.22-26
Women. Studies exclusively focused on women found that PTSD and depression may have damaging effects on physical health, particularly with increased risk for coronary heart disease related morbidity and mortality.27,28
Couples with someone who has PTSD. Comparative studies found that couples where one or both partners had PTSD experienced more severe conflict, greater anger, and increased cardiovascular reactivity to conflict discussions than couples where neither partner had PTSD. Anger and physiological stress responses to couple discord might contribute to CHD and heart disease risk within these relationships.29,30
Racial and ethnic minorities. Lastly, studies focused on racial or ethnic minority groups found that depression, stress, and anxiety due to disparities in social determinants of health,31 adverse childhood experiences,32 and racism/discrimination33-35 could place certain subpopulations at a higher risk for hypertension,32,33,35,36 cardiovascular reactivity,35 heart disease,31,34 and poor heart health outcomes.37
Read Also: Mediocre Medical Symptoms Of Anxiety
Ecg Leads I Ii And Iii
Leads I, II and III compare electrical potential differences between two electrodes. Lead I compares the electrode on the left arm with the electrode on the right arm, of which the former is the exploring electrode. It is said that lead I observes the heart from the left because its exploring electrode is placed on the left . Lead II compares the left leg with the right arm, with the leg electrode being the exploring electrode. Therefore, lead II observes the heart from an angle of 60°. Lead III compares the left leg with the left arm, with the leg electrode being the exploring one. Lead III observes the heart from an angle of 120° .
Leads I, II and III are the original leads constructed by Wilhelm Einthoven. The spatial organization of these leads forms a triangle in the chest which is presented in Figure 18, panel B.
According to Kirchhoffs law, the sum of all currents in a closed circuit must be zero. Since Einthovens triangle can be viewed as a circuit, the same rule should apply to it. Thus emerges Einthovens law:
How To Reduce Significant Artifact
A slight ECG artifact is not uncommon. However, you can reduce further interference through the following steps:
- Switch off non-essential electrical devices and equipment within the vicinity if possible.
- Check for cable loops and avoid running cables adjacent to metallic objects as they can affect the signal.
- Inspect wires and cables for cracks or breaks. Replace as needed.
- If possible, use surge suppressors with the power supply.
- Ensure that filters and preamplifiers are appropriately adjusted.
- Ensure securely connection between patient cable and the ECG device. Double check for gaps between connectors.
Also Check: Fear Of Really Long Words
Using Einthoven’s Triangle To Identify Lead Misplacements
Einthoven’s triangle can be helpful in the identification in incorrect placement of leads. Incorrect placement of leads can lead to error in the recording, which can ultimately lead to misdiagnosis.
If the arm electrodes are reversed, lead I changes polarity, causing lead II and lead III to switch. If the right arm electrode is reversed with the leg’s electrode, lead II changes polarity, causing lead I to become lead III, and vice versa. Reversal of the left arm and leg causes a change in polarity of lead III and switching of leads I and II.
Electrophysiological Basis Of The Ecg Leads
The movement of charged particles generates an electrical current. In electrocardiology the charged particles are represented by intra- and extracellular ions . These ions flow across cell membranes and between cells via gap junctions .
Electrical potential difference arise as the electrical impulse travels through the heart. Electric potential difference is defined as a difference in electric potential between two measurement points. In electrocardiology these measurement points are the skin electrodes. Thus, the electrical potential difference is the difference in the electrical potential detected by two electrodes.
In the previous discussion it was clarified how de- and repolarization generates electrical current. It was also explained that the electrical currents are conducted all the way to the skin, because the tissues and fluids surrounding the heart, indeed the entire human body, acts as electrical conductors. By placing electrodes on the skin it is possible to detect these electrical currents. The electrocardiograph compares, amplifies and filters the electrical potential differences recorded by the electrodes and presents the results as ECG leads. Each ECG lead is presented as a diagram .
Read Also: What’s The Phobia Of Throwing Up