Positive Symptoms Of Schizophrenia
In this case, the word positive doesnât mean good. It refers to added thoughts or actions that arenât based in reality. Theyâre sometimes called psychotic symptoms and can include:
- Delusions: These are false, mixed, and sometimes strange beliefs that arenât based in reality and that the person refuses to give up, even when shown the facts. For example, a person with delusions may believe that people can hear their thoughts, that they are God or the devil, or that people are putting thoughts into their head or plotting against them.
- Hallucinations: These involve sensations that arenât real. Hearing voices is the most common hallucination in people with schizophrenia. The voices may comment on the personâs behavior, insult them, or give commands. Less common types include seeing things that arenât there, smelling strange odors, having a funny taste in your mouth, and feeling sensations on your skin even though nothing is touching your body.
- Catatonia: In this condition, the person may stop speaking, and their body may be fixed in a single position for a very long time.
Many Individuals Who Develop Symptoms Of Schizophrenia When They Are 50 Years Of Age Or Older Exhibit A Rapid Decline Into Dementia However The Symptoms Of Older Schizophrenic Patients Who Do Not Develop This Rapid Decline In Their Mental Capacities Actually Improve Over Time
Edited By: Updated: Feb 23, 2010 05:55 IST2-Min Read schizophrenia dementia Alzheimer’s disease stroke
British Journal of Psychiatry,
DoctorNDTV is the one stop site for all your health needs providing the most credible health information,health news and tips with expert advice on healthy living, diet plans, informative videos etc. You can get the most relevant and accurate info you need about health problems likediabetes,cancer,pregnancy,HIV and AIDS,weight loss and many other lifestyle diseases. We have a panel of over 350 experts who help us develop content by giving their valuable inputs and bringing to us the latest in the world of healthcare.
Relative Specificity Testing By Comparing With Mci
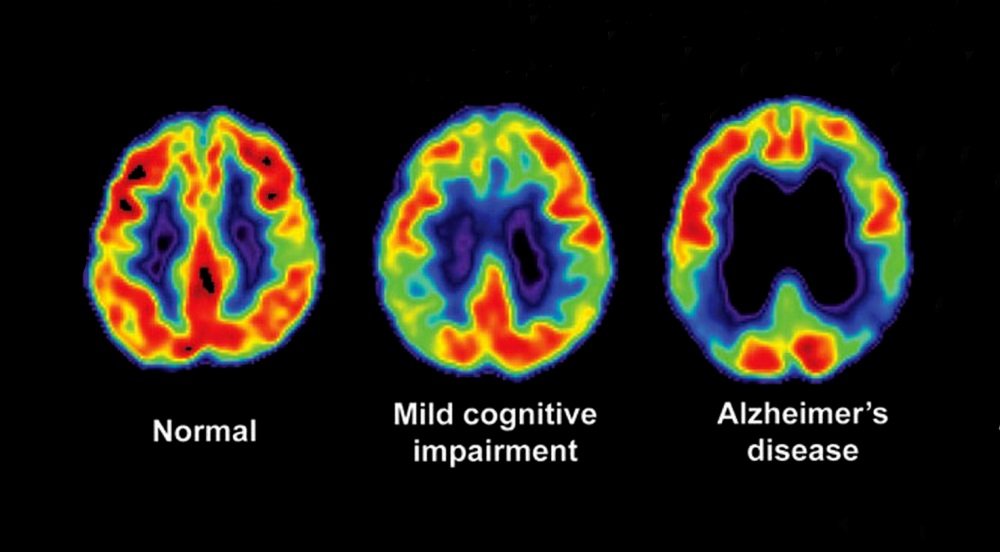
SZ patients also showed elevated RVI-MCI in both the discovery and replication sample . The ENIGMA SZ pattern of white matter deficits was not significantly correlated with those in MCI . The correlation between RVI-MCI and RVI-SZ was also significant but the r value was significantly smaller than the correlation between RVI-AD and RVI-SZ .
Also Check: Webmd Anxiety Disorder
Do People With Schizophrenia Develop Dementia
In his Lehrbuch der Psychiatrie of 1893, Kraepelin used the term dementia praecox for schizophrenia because of its onset in early life and the characteristic development of mental enfeeblement. He emphasised the progressive deterioration of cognition but noted that memory was spared. He distinguished this condition from paraphrenia in which cognitive impairment did not occur.
Over a century later, there is uncertainty about the course of cognitive function with ageing in schizophrenia. Early studies of the progression of dementia over the lifespan in individuals with schizophrenia have shown inconsistent results, although they were limited by a lack of standardised diagnostic criteria and specific evaluation techniques.
In a study of long-term in-patients with schizophrenia who had survived into old age, Reference Harvey, Parella and WhiteHarvey et al followed up a group for 30 months using the Clinical Dementia Rating . Over this period, 30% of the patients deteriorated, from a baseline of minimal or mild cognitive and functional impairment to impairments severe enough to warrant a secondary diagnosis of dementia.
Although many studies suggest a model of schizophrenia as a progressive dementing illness, others have supported the view that cognitive impairment in schizophrenia fits the model of a static encephalopathy .
Diagnosis And A Test For Schizophrenia
In men, schizophrenia symptoms typically start in their early- to mid-20s. In women, symptoms typically begin in their late 20s or early 30s. Some of the symptomswithdrawal, poor grooming habits, trouble focusingare common during teenage years, which can make diagnosis difficult.
While there is no specific test for the illness, a physician can conduct a psychological evaluation and medical exam to rule out other conditions like bipolar disorder or multiple personality disorder.
One challenge, Dr. Nucifora says, is that people with schizophrenia often lack awareness that their difficulties stem from a mental disorder. It often falls to family or friends to get them help. Early diagnosis and treatment can help improve the long-term outlook of the patient.
Understanding that the disease is long-term and that the symptoms will vary is helpful to both the family and patient.
Read Also: Was Audrey Hepburn Anorexia
Caveats On A Cellular
Given the ongoing dramatic changes in the distinction between neurons and glial cells in the brain, the above proposal that 4EC are pivotally involved in AD and schizophrenia defies the former notion that the targeted element can be conceptualized simplistically as neurons vs. macroglia vs. microglia, vs. other cells that are not of a neural lineage. In fact, considering the still unresolved nature of 4EC as precursors or variants of oligodendrocytes, their near-neuronal attributes and their features in common with conventional astrocytes, their postulated primary, even pathogenic, involvement in AD blurs the previously unassailable distinction among all conventional cell types in AD. Even if the present proposal about the predominant targeting of 4EC in AD does not survive experimental testing, it casts doubt on the ability to postulate targeting mechanisms based exclusively on neuronal vs. glial phenotypes. Thus, it is also possible that it is not specific cell types, but key attributes shared between neuronal and non-neuronal cells that are targeted early on in the disease process, if this process attacks first or in any way selectively neural cells. Similar considerations apply to schizophrenia, in which, as stated in the preceding section, the characterization of the possible participation of 4EC has barely begun solely by stating the possibility of such a mechanism.
Schizophrenia As The Graveyard Of Neuropathologists
Many believe that schizophrenia and related disorders result from alterations in brain circuits . Yet, this probably correct assumption lacks a concrete factual demonstration hundreds of unverified neuropathological claims non-withstanding and is in stark contrast with the relative wealth of information on the neuropathology of AD because virtually nothing claimed about histopathological observations in schizophrenia has survived efforts at independent verification or corroboration. This justifies Stevens admonition about schizophrenia being the graveyard of neuropathologists , which unfortunately continues to be the case decades since its enunciation. In fact, arguably the only widely accepted, consistent morphological alterations have been found by in vivo imaging, that consist in a reduction in gray matter, enlargement of the ventricles of the brain, and focal alterations in the white matter . This is hardly specific, much less pathognomonic, and is perhaps consistent with the increasingly popular syndromatic as opposed to a unique, or sole disease view of the disorder , which would be consistent with the lack of a truly unique and unanimously agreeable cellular and molecular neuropathology. Be that as it may, it justifies the still vaguely articulated perception that schizophrenia is a disease of the cerebral cortex .
Table 1. A simplified list of selected similarities and key differences between Alzheimers disease and schizophrenia.
Recommended Reading: What Is The Meaning Of Phobia
Alzheimer’s Disease Patients With Psychosis More Likely To Be Misdiagnosed Study Suggests
- Date:
- St. Michael’s Hospital
- Summary:
- People with Alzheimer’s disease who experience psychosis — including delusions and hallucinations — are five times more likely to be misdiagnosed with dementia with Lewy bodies compared to patients who do not, new research suggests.
People with Alzheimer’s disease who experience psychosis — including delusions and hallucinations — are five times more likely to be misdiagnosed with dementia with Lewy bodies compared to patients who do not, new research suggests.
Alzheimer’s disease is a type of dementia characterized by protein deposits in the brain including twisted fibers found inside brain cells. Dementia with Lewy bodies is believed to be caused by the buildup of a different abnormal protein aggregate found in nerve cells in the brain. Effective treatments for these conditions are still under development, but will almost certainly be different, according to the authors.
Researchers also found that Alzheimer’s disease was misdiagnosed in 24 per cent of all cases, with false positive and false negative rates both being 12 per cent. Previous research suggested that the rate of misdiagnosis in Alzheimer’s disease ranged from 12-23 per cent.
“An advantage of our study is that we used the final clinical diagnosis after years of follow-up, so the rate of misdiagnosis we described is the rate under ideal conditions,” she said.
Story Source:
Journal Reference:
Cite This Page:
Alzheimers Is A Brain Disease
People diagnosed with Alzheimers disease may display similar traits to those with mental illness. However, Alzheimers disease is more accurately defined as a brain disease, specifically, a progressive neurodegenerative condition. The American Psychiatric Association describes the brain disorder as a group of symptoms that lead to a decline in mental function severe enough to disrupt daily life.
The progression of the various stages of Alzheimers leads to memory loss, which affects ones ability to reason, learn, and make sound decisions. A person with Alzheimers can lose the ability to communicate effectively, and eventually, accomplishing simple daily activities becomes an overwhelming challenge.
Alzheimers disease is treatable, but not curable. Treating Alzheimers disease helps to slow its devastating progression and assists in providing quality of life through the multiple stages of the disease.
Dementia affects both mental and physical health, but it is not strictly defined as mental illness. Unlike mental illness, dementia is a disease that primarily affects seniors. Mental illness is nondiscriminatory and can be prevalent at any age. Yet while it differs from dementia, one in three seniors suffers from mental illness.
Don’t Miss: What Is The Phobia Of Throwing Up
Patterns Of Regional White Matter Deficits In Ad Mci And Sz
Five samples were analyzed to test the above hypothesesthe ADNI samples for AD and MCI and 3 SZ samplesa discovery sample from Baltimore, MD a replication sample from Beijing, China and a replication sample from the worldwide meta-sample from ENIGMA, which is the largest white matter imaging sample in SZ. Each sample had its own healthy controls. Details on sample size, demographic , and imaging information are in the Methods section and supplementary information. White matter microstructures were measured by FA of DTI. The ranks of regional FA effect sizes between patients and controls for each cohort are shown in and supplementary table S4. In AD, the largest effect sizes were in the fornix followed by the splenium of the corpus callosum . In MCI, the largest effect sizes were in the SCC and FX . In the 3 SZ cohorts, patients showed the largest effect sizes in the anterior corona radiata , anterior limb of the internal capsule , FX, and body of the corpus callosum . The regional patient-control effect sizes in the discovery and replication cohorts were significantly correlated with those reported by ENIGMA .
Risk For Dementia Is Increased For Individuals With Schizophrenia
Schizophrenia is a chronic disorder characterized by symptoms that include hallucinations, delusions, abnormalities in the verbal expression of thought, diminished social interactions, diminished motivation, and difficulties with cognitive tasks involving attention, memory, and planning. The long term course of this disorder varies. Some individuals, with the help of appropriate medication and social support, can live independently, be employed, and enjoy friends and hobbies. For others, however, the symptoms are difficult to manage and interfere with most aspects of their lives, often leading to disability and early death. It is also not uncommon for persons with schizophrenia to use street drugs and alcohol, and chronic abuse of alcohol or illicit drugs negatively impacts their long-term outcome.
Although cognitive symptoms involving attention and memory are common in persons with schizophrenia, such symptoms tend to be stable and non-progressive through middle age. Whether schizophrenia is associated with an increased risk for a progressive dementia later in life has been the focus of several research studies, but the results so far have been inconclusive. Prospective studies addressing this issue are difficult to perform given the need for a large study population and the long period of time between an initial diagnosis of schizophrenia and the onset of dementia.
You May Like: Anxiety Causes Fainting
What Is Schizophrenia Regression
When following a properly regimented medication plan, avoiding mind- or mood-altering substances, and productively dealing with underlying trauma, schizophrenia regression is rare. Many individuals experience improved quality of life as long as they follow their treatment program.
However, if someone is following their treatment plan and symptoms suddenly become worse, it could be a sign of schizophrenia regression, and the approach to treatment may need to be adjusted. It can be challenging to find the best type or dosage of schizophrenia medication for each individual, and if symptoms dont improve, its important to talk to the prescribing doctor about other options before choosing to end treatment altogether.
Some individuals diagnosed with schizophrenia may choose to discontinue treatment, believing that theyre better or no longer need medication or help. When that happens, the symptoms often return and may even grow worse. The best option is to stay the course and adjust treatment approaches as needed. Once the individual has achieved a stable baseline, they simply have to take maintenance medication to live a balanced life.
Also Check: Dementia Vs Senility
Trouble Keeping A Job
Symptoms like hallucinations, delusions, and scattered thinking can make it hard to hold a job. People with schizophrenia are six to seven times more likely to be unemployed than those without this condition.
Working is important for many reasons. Not only does having a job let you support yourself, it also gives you a feeling of self-worth.
You’ll be more likely to find and keep a job if you can get on a treatment to manage your symptoms. If you already work, you may qualify for job accommodations — things that make it easier to do your work — under the Americans with Disabilities Act .
Helpful accommodations for schizophrenia include:
- A flexible schedule
- Counseling
You May Like: Is Celine Dion Anorexic
Mental Illness Tied To Increased Dementia Risk
Batya Swift Yasgur, MA, LSW
Mental disorders in early life are associated with a significantly increased risk of dementia in later years.
Results of a large, longitudinal, population-based study show that individuals hospitalized for a mental health disorder had a fourfold increased relative risk for developing dementia compared to those who were not hospitalized with a mental illness.
In addition, those with dementia plus a mental disorder developed dementia almost 6 years earlier than those without a mental illness.
The findings were consistent among men and women, in patients with early- and late-onset dementia, in those with Alzheimers and non-Alzheimers dementia, and across all mental health disorders and remained so after accounting for preexisting physical illness and socioeconomic factors.
Dementia is not typically treated until later in life, but our study suggests that we need to be thinking about dementia prevention much earlier in the life course, study investigator Leah Richmond-Rakerd, PhD, assistant professor, Department of Psychology, University of Michigan, told Medscape Medical News.
Supporting young peoples mental health could be a window of opportunity to help reduce the burden of dementia in older adults, she said.
The findings were February 16.
Also Check: Does Pristiq Work For Anxiety
Mental Illness And Dementia: Similarities And Differences
In many ways, mental illness can manifest the same symptoms of dementia, and vice versa. While there are a lot of similarities between the two, there are also some pretty critical differences. If you have a loved one in hospice in San Francisco and elsewhere who is suffering from one of the two, youll want to read on. To recognize Mental Illness Awareness Week , we will use this blog to explain the similarities and differences between mental illness and dementia.
Each year, millions of Americans live with a mental health condition, but its important to remember that mental illness affects everyone either in a direct or indirect way through friends, family or coworkers, according to the National Alliance on Mental Illness . Despite the reach and prevalence of mental illness, though, stigma and misunderstanding are still widespread. Couple that misunderstanding with the fact that mental illness can imitate the symptoms of dementia, and vice versa, and you have a serious, pervasive problem in this country.
Also Check: Can High Blood Sugar Cause Anxiety Attacks
Increased Risk Of Dementia In Individuals With Schizophrenia
The finding of no familial coaggregation between schizophrenia and Alzheimer’s dementia is conflicting with the growing body of literature emerging of an intriguing relationship between schizophrenia in the individual and the development of dementia . However, whereas most of the studies investigating coaggregation used Alzheimer’s dementia as the main outcome measure, the studies investigating schizophrenia in the individuals themselves used all-cause dementia .
Does Adhd Medication Lead To Schizophrenia
Some people who use stimulant medication to relieve the symptoms of ADHD go on to experience symptoms of psychosis.
However, it is unclear whether using stimulants to treat ADHD increases the risk of schizophrenia or schizophrenia-type symptoms, specifically psychosis. These symptoms may have appeared without the use of stimulant medication.
Exposure to psychostimulant drugs does appear to increase the risk of psychosis. Psychosis that appears at a younger age is more likely to result from the use of psychostimulant drugs.
However, it remains unclear whether psychosis results from the use of the drugs or whether these individuals were already susceptible to psychosis.
In addition, the type of psychosis that people with ADHD experience tends to be different from that in people with schizophrenia as it involves brief mental changes rather than full hallucinations.
The symptoms of ADHD and schizophrenia are different, but they overlap in the area of inattention.
Don’t Miss: Spasmenagaliaphobia