What Is A Diagnosis
A diagnosis is a formal label that describes a certain set of problems or symptoms. Official diagnostic criteria describe which symptoms are necessary for any particular diagnosis. A diagnosis should help the person experiencing symptoms and should always be used in the context of a wider understanding of the persons needs, challenges and strengths when developing care plans. In mental health, diagnoses often describe a group of shared thoughts, behaviours and symptoms. Identifying these groupings helps professionals communicate effectively and, more importantly, supports research to identify what works to help people experiencing difficulties.
In some cases, a persons particular profile of difficulties may not meet the threshold for a diagnosis, but they can still be very distressing and warrant treatment.
There are two similar but not identical, recognised sets of diagnostic criteria for mental health problems:
- The International Classification of Diseases 11th Revision produced by the World Health Organisation .
- The Diagnostic and Statistical Manual 5th Edition produced by the American Psychiatric Association .
People find different kinds of meaning in diagnosis. For some people it helps them explain or make sense of the experiences they have had and the impact it has had on their lives. For others it may feel stigmatising, reductive, meaningless or result in them feeling like they are being treated as a set of symptoms rather than a person.
Prevalence Of Cptsd And Ptsd
Research on the prevalence of CPTSD and PTSD in different countries, cultures and settings has just begun. This work has been substantially aided by the development of a validated self-report measure for ICD-11 PTSD and CPTSD, the International Trauma Questionnaire Reference Cloitre, Shevlin, Brewin, Bisson, Roberts and Maercker5 and a clinician interview, the International Trauma Interview for which reliability and validity data are accumulating. Factor analyses across different countries and cultures have consistently conformed with the conceptualisation of CPTSD as comprised of two symptom clusters, namely symptoms of PTSD and of disturbances in self-organisation. General population studies using the ITQ indicate that in high-income countries such as the USA, the UK, Germany and Israel the rates of PTSD and CPTSD combined range from 2.0 to 12.7%, whereas in the low-income countries studied thus far in Africa , rates of the two disorders are higher ranging from 30.6 to 37.0%.
What Helps With Ptsd And Complex Ptsd
There are two particular interventions that are generally recommended if a child or young person has a diagnosis of PTSD : Trauma-focused Cognitive Behavioural Therapy and Eye Movement Desensitisation and Reprocessing . Research has consistently found that these are effective for PTSD in children and young people. However that does not mean that they will work for all children with PTSD and some research indicates that other approaches might also be effective .
There is much less research evidence about what interventions are effective for Complex PTSD, however there is emerging evidence that what works for PTSD is likely to be effective for Complex PTSD , but it may require more sessions and more focus on developing a trusting relationship .
References:
Recommended Reading: 3 Stages Of Schizophrenia
Assessment Of Complex Trauma In Children
Children exposed to complex trauma often evidence impairment in several domains.Cook and others describe symptoms and behavioural characteristics in seven domains:
Trauma History and Caretakers
Trauma-Related Symptoms
Development & Social/Emotional Functioning
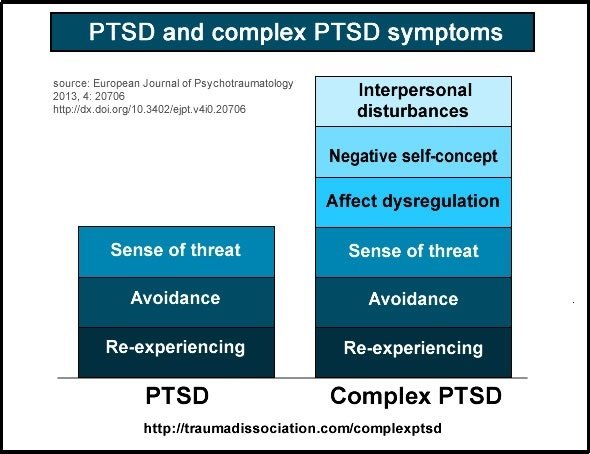
Definition Of Cptsd Versus Ptsd
The ICD-11 formulation and characterisation of the two disorders follow from a long history of clinical observation that individuals who experienced chronic, repeated and prolonged traumas, such as childhood sexual abuse or domestic violence, tended to experience more complex reactions extending beyond those typically observed in PTSD and which included effects in three key domains: emotion regulation, self-identity and relational capacities. Thus, in ICD-11, CPTSD is a disorder that includes not only the symptoms of PTSD but additionally disturbances in the three above domains.
The ICD-11 formulation of PTSD requires exposure to a trauma defined as an extremely threatening or horrific event or series of events. Similar to the original DSM version of PTSD, the disorder includes three core elements or clusters: re-experiencing of the traumatic event in the present, avoidance of traumatic reminders and a sense of current threat. This formulation conceptualises PTSD primarily as a conditioned fear response and the re-experiencing and avoidance symptoms are specifically tied to the traumatic event. CPTSD includes the three core elements of PTSD as well as three additional elements called disturbances in self-organisation that are pervasive and occur across various contexts: emotion regulation difficulties , negative self-concept and relationship difficulties .
You May Like: What Is The Fear Of Feet Phobia Called
Ptsd: Screening & Assessment
;is a 20-item self-report tool that corresponds to the 20 symptoms listed in DSM-5 . It can provide a global assessment of PTSD severity both at the time of diagnosis and over the course of treatment.;
On a 4-point scale, scores can be tabulated for individual items to give information about the severity of the four DSM-5 symptom clusters. If a score of 2 is considered to be a positive endorsement of a given criterion, the PCL-5 can be used in combination with a clinical interview to make a provisional DSM-5 diagnosis. Testing the PCL-5 with veterans has determined a score of 31 to 33 to be a valid cutoff for a positive screen, but more work is necessary to validate this score in civilian populations .;
Dissociative Experiences Scale
Because the DSM-5 incorporates a dissociative subtype of PTSD, it is useful to screen for dissociative symptoms, which are not captured by the PCL-5.
The self-report;Dissociative Experiences Scale ;asks respondents to rate what percentage of the time they experience a given dissociative symptom . The general population average is 4 to 8 percent compared with 26 to 42 percent among people with PTSD . The DES cannot be used for diagnosis, but scoring over 20 per cent indicates the need to further explore dissociative symptoms .
Complex Ptsd: How A New Diagnosis Differs From Standard Ptsd
- 4 minute read
Your palms sweat. Your heart races. You dont remember where you are are you here, now, or back in another, scarier time?
This is a flashback. And for many people living with PTSD, its a common experience. Faced with a reminder of a traumatic event, someone with PTSD can be jerked back into the mental, emotional and even physical experience of trauma.
But what happens when that trauma is ongoing, or a prolonged series of events? This is where a Complex PTSD diagnosis bridges an important behavioral health gap.
Don’t Miss: What Is A Phobia Of Spoons Called
Post Traumatic Stress Disorder
Post traumatic stress disorder describes symptoms associated with a traumatic event such as a car accident, witnessing violence, natural disaster, etc . The symptoms may include recurrent bad dreams, physical reactions, flashbacks, startle reaction, loss of interest in usual activities, avoiding reminders of the event, etc. To address developmental influences, ZERO TO THREE has included language in their Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood Revised that can supplement the adult focused Diagnostic and Statistical Manual of Mental Disorders . Currently, the diagnosis of Posttraumatic Stress Disorder in Preschool Children is under consideration for the DSM 5th edition which is due for publication in 2013 . The DC:0-3 and the proposed revised diagnosis include additional developmentally-based, diagnostic criteria for PTSD in young children.
Other Terms For Complex Ptsd
Complex PTSD is a fairly new term. Professionals have recognised for a while that some types of trauma can have additional effects to PTSD, but have disagreed about whether this is a form of PTSD or an entirely separate condition, and what it should be called.
For example, you may find some doctors or therapists still use one of the following terms:
- enduring personality change after catastrophic experience
- disorders of extreme stress not otherwise specified this term is more common in America than the UK.
“At times I felt nothing was going to end the distress, experiencing more than 10 flashbacks a day… It was a long process of recovery, with lots of bumps along the road, but the right medication and long-term therapy with someone I came to trust, has changed my life.”
Don’t Miss: What Is The Fear Of Spoons Called
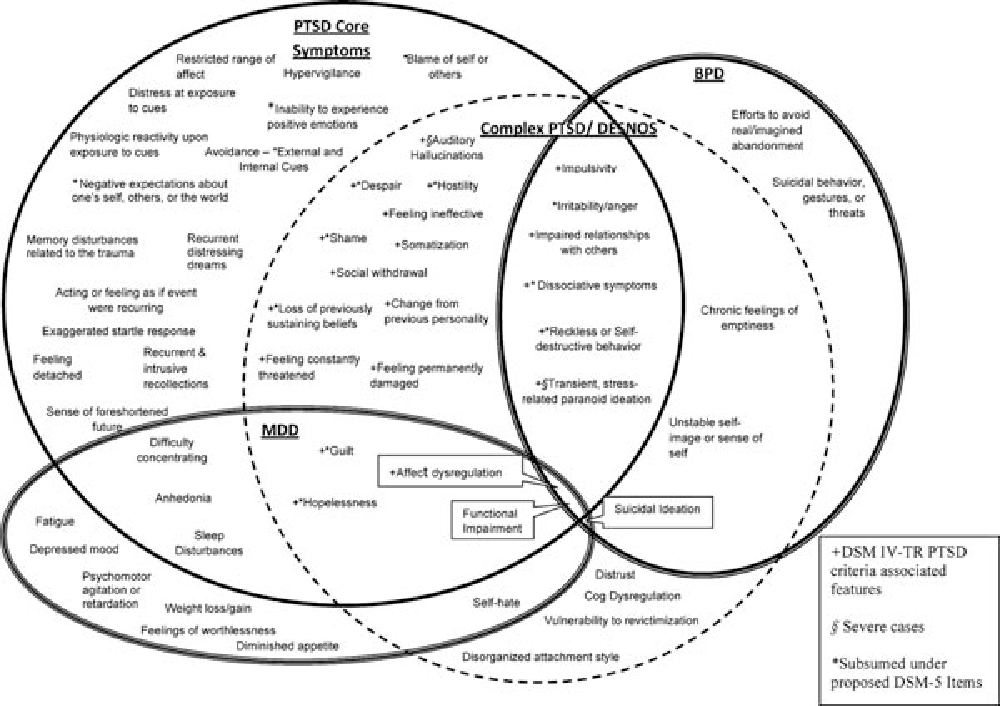
Cptsd And Borderline Personality Disorder
There has been debate over nearly two decades as to whether CPTSD is actually PTSD with comorbid borderline personality disorder . Several studies using various statistical techniques have demonstrated that individuals with CPTSD are distinguishable from those with BPD. There are several notable clinical differences that have treatment implications. Individuals with CPTSD experience a severe but stable negative self-concept whereas those with BPD report shifts in their self-image vacillating between highly positive and highly negative self-perceptions. CPTSD relational difficulties are characterised by a tendency to avoid and have difficulty maintaining relationships, particularly during periods of conflict or high emotion whereas BPD is associated with rapid engagement followed by ups and downs or idealisation and devaluation of relationships. Although emotion regulation difficulties are central to both CPTSD and BPD, their expression can be quite different with suicide attempts and gestures and self-injurious behaviours a core feature and a first target of treatment for BPD in contrast to CPTSD, which does not include either problem for diagnosis and preliminary data indicate rates of these problems are substantially lower in CPTSD relative to BPD.
How Do I Know I Am In A Flashback
We can often find ourselves in a flashback without ever having seen the flash. There are a variety of clues that we can learn to identify as signs that we are caught in a flashback. This is essential to recovery, as naming our experience flashback often immediately brings some relief, and more importantly point us in the direction of working the other 12 steps of flashback management .
One common clue that we are in a flashback occurs when we notice that we feel small, helpless, hopeless and so ashamed that we are loath to go out or show our face anywhere.
| return to top |
Recommended Reading: How Are Areas Of Depression Represented On A Topographic Map
How Do I Discuss This With My Doctor
First, have a look at the symptoms list in the beginning of this article and highlight the ones that you feel applies to you. Then, for each highlighted item, list a few examples to show how that particular symptom manifest itself in your life, and what impact it is having on your quality of life.
Your doctor would be naturally attuned to the use of symptom keywords, and he would be keenly interested to hear how these symptoms present themselves in your daily life.
In addition to the symptoms listed above, which are specific to Complex PTSD, you may also find it helpful to look at the following list of symptoms that are common to both conditions:
- Re-experiencing
Remember, it is dangerous to self-diagnose. So focus on your symptoms and experiences, and let your doctor do the diagnosis. You may also find the International Trauma Questionnaire helpful.
Treatment Of Complex Ptsd
An important debate has been taking place over whether complex PTSD requires a different kind of psychological treatment to PTSD. The International Society for Traumatic Stress Studies produced a position paper recommending three stages or phases of treatment, each with a distinct function. Phase 1 focuses on ensuring the individual’s safety, reducing symptoms, and increasing important emotional, social and psychological competencies. Phase 2 focuses on processing the unresolved aspects of the individual’s memories of traumatic experiences so that these are integrated into an adaptive representation of self, relationships and the world, using standard or slightly adapted methods taken from conventional trauma-focused cognitivebehavioural therapy. Phase 3 involves consolidation of treatment gains to facilitate the transition from treatment into a greater engagement with the outside world.
BOX 3 NICE recommendations for trauma-focused cognitivebehavioural interventions for CPTSD
Also Check: What Is The Meaning Of Phobia
Recovering From Ptsd By Regaining Self
Posted June 16, 2013
In the DSM-5 released in May, PTSD just got more complex. It added a new symptom domain of “negative alterations in cognitions or mood,” and expanded the hyperarousal domain to include aggressive, reckless, or self-destructive behavior. It also added a sub-type characterized by dissociation . These changes reflect advances in science and clinical practice, which echo what trauma survivors have been saying for decades : PTSD is a radical shift from normal self-regulation to being trapped in a constant state of alarm.
Mobilization is essential to experiencing pleasurable excitement, enthusiasm, and achievement. But too much mobilization for too long leads to tension, frustration, recklessness, and even self-harm. Similarly, when the body and brain re-group, this can produce pleasurable and healthy states of relaxation, calm, and mindful acceptance. However, when re-grouping becomes extreme and persistent, the result can be emotional shut-down and exhaustion, depression, despair, or dissociation. Self-regulation is the constant balancing act between mobilization and re-grouping that enables us to be optimally effective and to feel true satisfaction.
Re-setting the brain’s alarm requires seven steps, which are at the heart of every effective treatment for PTSD despite their many differences:
Complex Ptsd Bpd And Personality Disorders
Recent research has produced detailed analysis of the symptoms of Complex PTSD, PTSD and Borderline Personality Disorder . Many people with BPD either have PTSD, or meet the proposed diagnostic criteria for Complex PTSD. Complex PTSD was shown to be a separate diagnosis from Borderline Personality Disorder because a significant number did not meet the diagnostic criteria for BPD . In 1992, when first proposing Complex PTSD, Judith Lewis-Herman stated:
Concepts of personality developed in ordinary circumstances are frequently applied to survivors, without an understanding of the deformations of personality which occur under conditions of coercive control. Thus, patients who suffer from the complex sequelae of chronictrauma commonly risk being misdiagnosed as having personality disorders. They may be described as “dependent,” “masochistic,” or “selfâdefeating.”Earlier concepts of masochism or repetition compulsion might be more useâ fully supplanted by the concept of a complex traumatic syndrome.:388
Also Check: What Does The Suffix Phobia Mean
Is Complex Ptsd A Separate Condition
The International Classification of Diseases identifies complex PTSD as a separate condition, though the DSM-5 currently does not.
Complex PTSD is a relatively recent concept. Because of its variable nature, healthcare professionals may instead diagnose another condition. They may be especially likely to diagnose borderline personality disorder .
Some researchers have areas of substantial overlap between complex PTSD and BPD.
However, the conditions may also have differences. Authors of a study from 2014 reported that, for example, people with complex PTSD had consistently negative self-conceptions, while people with BPD had self-conceptions that were unstable and changing.
People with complex PTSD may experience difficulties with relationships. They tend to avoid others and may feel a lack of connection.
BPD can cause a person to swing between idealizing and undervaluing others, resulting in relationship difficulties.
It is possible for a person with BPD to also experience complex PTSD, and the combination may result in additional symptoms.
A person with complex PTSD may experience symptoms in addition to those that characterize PTSD.
Common symptoms of PTSD and complex PTSD include:
People with PTSD or complex PTSD may also experience:
Symptoms of complex PTSD can vary, and they may change over time.
People with the condition may also experience symptoms that are not listed above.
Are Treatments Different
Treatments for PTSD and C-PTSD are similar. The main treatments are psychotherapy, medication, or a combo of both.
Therapy for PTSD and C-PTSD can help you learn more about your trauma and how it affects you. Therapy can also help you develop coping skills for triggers and give you tools to manage your symptoms.
For some, medication such as antidepressants may also be helpful to manage symptoms.
One difference between the two mental health conditions is that those living with C-PTSD may need long-term therapy and support to recover. Theres also an emphasis on forming a strong therapeutic alliance.
Also Check: Can Depression Make You Lose Your Appetite
What Is Complex Post
by Shirley Davis | Sep 3, 2019 | CPTSD Research, What is CPTSD |
Most people have heard of post-traumatic stress disorder that afflicts many men and women returning from a war zone. It is characterized by flashbacks, unstable mood, and survivors remorse. However, many have never heard of a condition that often develops in childhood and changes the course of the childs life forever, complex post-traumatic stress disorder .
For a good definition of CPTSD, we turned to Beauty After Bruises, an organization that offers outreach focused on adult survivors of childhood trauma who have complex PTSD with or without the presence of a dissociative disorder. Their definition of complex post-traumatic stress disorder as follows:
CPTSD forms in response to repeated interpersonal violence that leaves the victim, a child or adult, feeling trapped with no hope of escape or of imminent death.
Complex post-traumatic stress disorder is a developmental trauma disorder which is wildly different than post-traumatic stress disorder that normally, but not always, forms in adulthood.
The trauma model states that children who experience chronic sexual, psychological, physical abuse and neglect develop CPTSD. However, it also forms in kids who suffer slavery, human trafficking, working in sweatshops, war or survivors of concentration camp environments and cults. The trauma which causes this disorder may also include having experienced betrayal, defeat, and shame.