Can Ptsd Cause Bipolar Disorder
Although little evidence points to PTSD as a direct cause of bipolar disorder, experts do recognize links between the two conditions.
Its not clear what causes bipolar disorder, but a combination of brain chemistry/structure, genetics, and environmental factors may play a role.
One major environmental trigger? Stressful events, such as:
- moving away from home
- going through a breakup
- dealing with challenges at work
Traumatic events can also cause stress both in the moment and later, while you work to recover from the experience.
Not everyone who experiences trauma goes on to develop PTSD, bipolar disorder, or any mental health condition. That said, the lingering stress of a traumatic experience can factor into mental health symptoms, including anxiety and depression. Repeated childhood trauma also increases your chances of developing complex PTSD .
How Are Ptsd And Bipolar Disorder Similar And How Are They Different
PTSD and bipolar disorder have their similarities and differences. However, it has been found that up to 40% of those with bipolar disorder also meet the diagnostic criteria for PTSD.
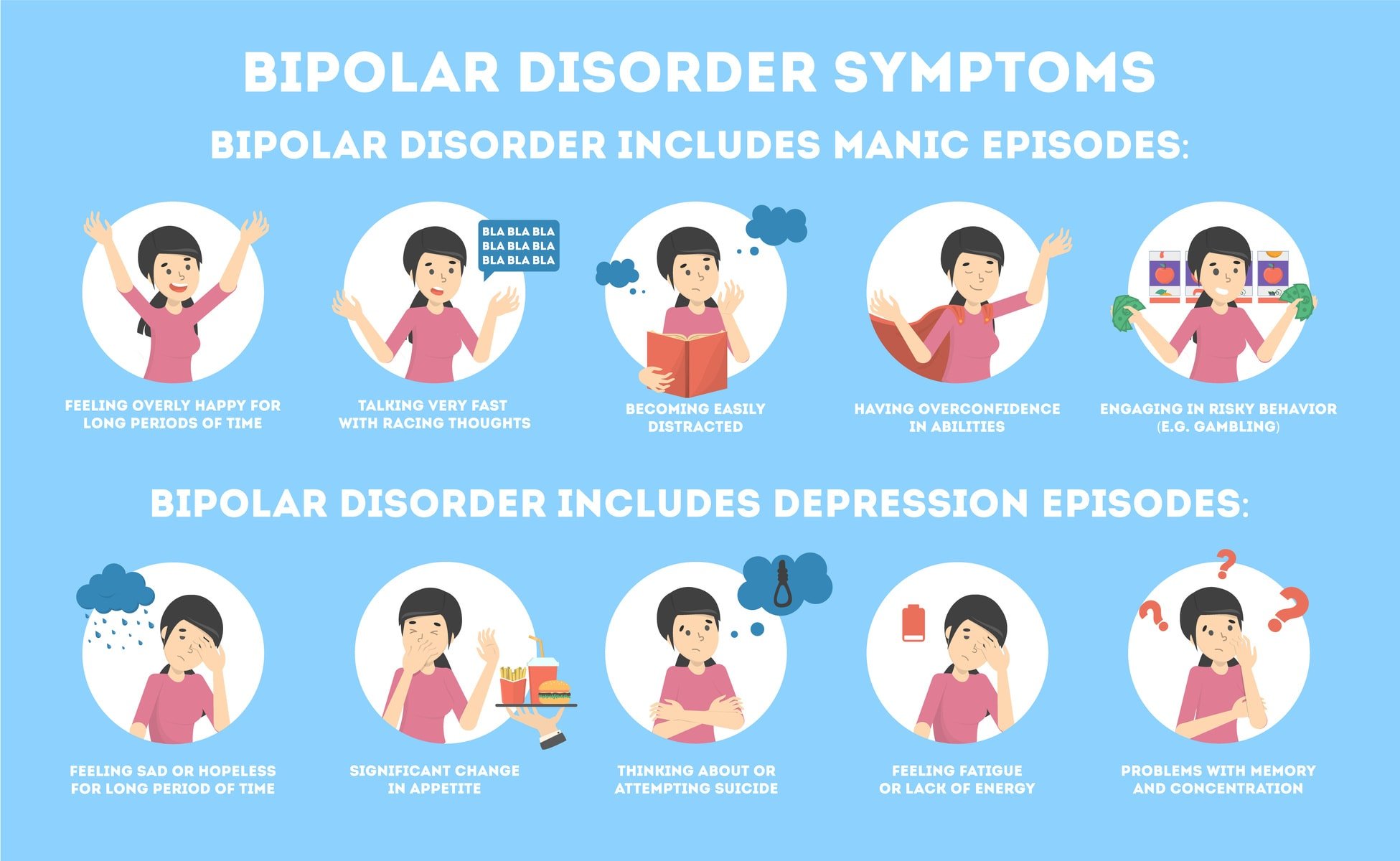
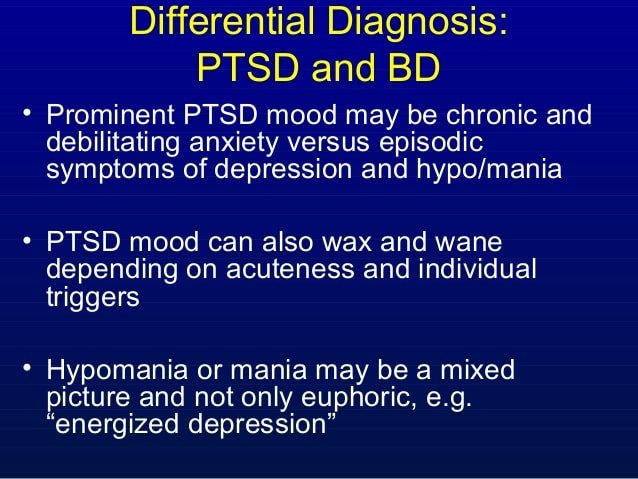
Lets start with similarities first. PTSD and depressive episodes can have very similar symptoms at times. Not only can both force you to lose interest in things you used to regularly enjoy, but they can also provide a certain amount of emotional numbness. Irritability and emotional outbursts can also be prevalent in both.
In regards to PTSDs similarities with manic episodes, both people with PTSD and bipolar disorder can experience paranoia, and nightmares are possible. Like some with PTSD, those with bipolar disorder experiencing a manic episode may have trouble concentrating, however it is for different reasons. For those with PTSD, it can be due to the after-effects of the trauma, but for those experiencing a manic episode, it can be due to racing thoughts.
PTSD does not have the extreme emotional mood shifts the way bipolar disorder does.
How To Understand If You Were Misdiagnosed With Bipolar Ii Disorder
There are several questions you can ask yourself to understand whether you were wrongfully diagnosed with bipolar II disorder.
1. Did you have bipolar symptoms prior to taking psychiatric medication?
In other words, think about your life from an objective perspective. Did you have periods of hypomania followed by periods of depression ? If you did, well then your diagnosis is likely correct, however if you never had these symptoms prior to taking medication, you may be a victim of misdiagnosis.
2. Do you really have a history of hypomania?
Many people who are misdiagnosed with this mental illness do not have a history of hypomania. The hypomania may have been induced by a traumatic experience and/or medication that they took. Certain people who are resistant to depression treatments may continue trying medications and find no relief. A psychiatrist may then experiment with drug combinations that may trigger hypomania-esque symptoms.
3. Do any immediate relatives have bipolar disorder?
If immediate relatives have bipolar disorder, your chances of also having it significantly increase. First determine whether there are any people in your immediate family with a bipolar diagnosis. Then think about whether any blood-relatives have the illness. Assuming no relatives have the illness, the odds that you have it are less likely.
4. Have you suffered any sort of trauma?
5. Do symptoms occur in homeostasis?
6. Do you use illicit drugs?
7. How frequent are your mood cycles?
Don’t Miss: How To Get Motivated To Exercise When Depressed
How Are Bipolar Disorder And Ptsd Different
The symptoms of bipolar disorder and PTSD can seem similar. Yet there are plenty of differences between the two conditions, both in the symptoms themselves and the patterns they take.
First, bipolar disorder falls into the category of mood disorders, so the symptoms you experience mainly relate to your mood and emotions. Theyll also appear in distinct episodes typically marked by significant changes in mood and energy.
These episodes of mania, hypomania, depression, or a combination of these symptoms can last from a few days to a few weeks, though depression can persist for a longer period of time. Between these episodes, you may not experience any symptoms at all.
As for PTSD, the new edition of the Diagnostic and Statistical Manual of Mental Disorders categorizes the condition as a trauma- and stressor-related disorder. In other words, you wont develop PTSD unless you experience some kind of trauma.
PTSD usually wont involve these key symptoms of mania:
- a high mood state characterized by heightened energy or euphoria
- increased self-esteem, self-absorption, or grandiosity
- pressured or confusing speech
- feeling refreshed on little sleep
It often does, however, involve an irritable mood, along with impulsivity or a tendency to take risks symptoms that commonly appear with mania.
PTSD also involves other trauma-specific symptoms, including:
Impact Of Ptsd On Bipolar Disorder
Having PTSD along with bipolar disorder can have a major negative impact on your life. People with PTSD and bipolar disorder appear to have more problems across a number of different areas in their lives.
For example, PTSD has been found to worsen the quality of life for people with bipolar disorder. A 2010 study found that patients with co-occurring bipolar disorder and PTSD experienced more rapid cycling periods and increased risk for suicide attempts.
If you are having suicidal thoughts, contact the National Suicide Prevention Lifeline at 1-800-273-8255 for support and assistance from a trained counselor. If you or a loved one are in immediate danger, call 911.
For more mental health resources, see our National Helpline Database.
Finally, PTSD has also been found to be associated with greater levels of depression among people with bipolar disorder, according to a 2013 study.
Also Check: What Is The Meaning Of Phobia
Learn The Differences Between These Two Disorders How To Spot The Signs Of Each And How To Treat Them
Life is turbulent, and changing moods can often be a natural response to stressful situations.
But for some, mood shifts are so extreme that they could be a sign of more serious conditions such as borderline personality disorder and bipolar disorder, both of which are characterized in part by major mood swings, according to Frank Yeomans, M.D., Ph.D., director of training at the NewYork-Presbyterian Borderline Personality Disorder Resource Center, an internationally recognized center for the study of personality disorders, and a clinical associate professor of psychiatry at Weill Cornell Medicine Department of Psychiatry.
This partial similarity in mood shifts, going from an extremely high mood to a very low mood, causes many people, including some clinicians, to confuse the two disorders, says Dr. Yeomans, who is also an adjunct associate professor of psychiatry at the Columbia University Vagelos College of Physicians and Surgeons Center for Psychoanalytic Training and Research. Yet they are two distinct and serious diagnoses with different symptoms that require different methods of treatment.
Both illnesses affect millions of Americans. Bipolar disorder is estimated to affect 2.8 percent, or roughly 6.5 million adults, according to the National Institute of Mental Health. The prevalence of borderline personality disorder is estimated to range from 1.6 to 5.9 percent of the American adult population.
What Causes Complex Ptsd
The types of traumatic events that can cause complex PTSD include:
- childhood abuse, neglect or abandonment
- ongoing domestic violence or abuse
- repeatedly witnessing violence or abuse
- being forced or manipulated into prostitution
- torture, kidnapping or slavery
- being a prisoner of war.
You are more likely to develop complex PTSD if:
- you experienced trauma at an early age
- the trauma lasted for a long time
- escape or rescue were unlikely or impossible
- you have experienced multiple traumas
- you were harmed by someone close to you.
“Developing PTSD after experiencing domestic violence was not something I was prepared for. Physically I left my old home. Mentally I am still there. The prison is no longer that house it is my mind. My thoughts. My memories.”
Misdiagnosis with BPD
Some of the symptoms of complex PTSD are very similar to those of borderline personality disorder , and not all professionals are aware of complex PTSD.
As a result, some people are given a diagnosis of BPD or another personality disorder when complex PTSD fits their experiences more closely. Professionals disagree about when it’s helpful to diagnose someone with a personality disorder or when another diagnosis or description is better. To find out more see our page on why personality disorders are controversial?
See our pages on borderline personality disorder and personality disorders for more information on these diagnoses.
Read Also: What Is The Phobia Of Storms Called
Common Ptsd Myths Debunked
Often, injury leads to chronic pain. About one in three people in the U.S. experience chronic pain in their lifetime. In one small study, out of 20 people who had experienced chronic pain after a car accident, 50 went on to develop PTSD.
Beyond chronic pain, PTSD can play a role in other physical conditions. A review published in 2010 looked at a range of conditions from psychological to physical that are comorbid with PTSD. The authors found that over the past decade or so, more research has been done to look at PTSDs relationship to everything from hypertension to obesity.
The authors cite one example of people two months after they survived the 9/11 terror attacks. These people showed an increase between 1.7 millimeters and 3.3 mm of mercury of systolic blood pressure compared with the year before. For this specific population, trauma exposure appeared to greatly increase blood pressure levels.
What You Should Do
What do you do if you believe you have been misdiagnosed by a mental health professional? The first thing to do is not to panic. Although we look up to doctors, they are the only people with diplomas. They are fallible and sometimes make mistakes such as giving the wrong diagnosis. If you feel your doctor has made a mistake, ask for a second opinion outside of that doctors clinic. Most insurance companies allow this maneuver and even if yours does not it is worth the peace of mind.
Second, make sure to be totally upfront and honest with your clinician. A mental health professionals diagnosis is only as good as the information you give them. If you hold back facts from your childhood or other information you are hurting yourself and become more likely to be misdiagnosed.
Last, if you do not feel your mental health professional is a good fit and that your diagnosis is wrong, seek out someone else for help. Take advantage of websites that help you find specialists who deal with complex post-traumatic stress disorder to find a good match.
Misdiagnosing CPTSD as bipolar disorder is dangerous and will not help the person experiencing symptoms to heal. Definitely, reach out to a mental health professional when you need help but keep in mind that misdiagnosis can and does occur.
Believe in yourself. You are braver than you think, more talented than you know, and capable of more than you imagine. ~ Roy T. Bennett
Don’t Miss: What Is The Meaning Of Phobia
Pmdd Symptoms Can Mimic Those Of Depression Anxiety Ptsd And Other Disorders
As you can see, the symptoms of PMDD are no joke. In fact, almost all PMDD symptoms are identical to those experienced by people with anxiety disorders, major depression, post-traumatic stress disorder, bipolar disorder, borderline personality disorder, and a few others.
In a sense, this isn’t all that surprising. Since PMDD is caused by a hormonal imbalance, and hormones are made up of chemicals, PMDD is technically caused by a chemical imbalance â just like any other mood disorder. Still, a mental health misdiagnoses isn’t something to take lightly, because both depression and severe PMDD can be life-threatening.
Hypomania Can Go Unnoticed
Some people with bipolar II who present to clinicians do not have a clear history of hypomania.
What is Hypomania?
Hypomania refers to an elevation in mood that is less drastic than mania. Hypomania may sometimes be enjoyable due to the increased energy and confidence that often come with it. However, it can still lead to impulsive behaviour with adverse consequences, such as overspending and damaging personal relationships. Because it is more subtle in how it is experienced, it is harder to pick up.
Because it is enjoyable, people with bipolar II may not seek treatment during a hypomanic episode. Research suggests that people with bipolar II are more likely to seek treatment for a depressive episode than a hypomanic episode. Hypomania also does not tend to involve psychotic symptoms , or a serious break from reality. Furthermore, hypomania does not tend to end in hospitalisation, as mania sometimes does.
Hypomania is therefore less likely to be recognised by mental health professionals, the person with h bipolar II or their family and close friends. This could explain the research finding that misdiagnosis of bipolar disorder as unipolar depression is more common in bipolar type II than in bipolar type I7.
Don’t Miss: What Is The Meaning Of Phobia
Differential Diagnosis: Bipolar Disorder Vs Adhd
Clinicians working to differentiate between ADHD and bipolar disorder should conduct a comprehensive, clinical interview that aims to determine whether the following unique signs of bipolar disorder are present:
- Unlike ADHD, symptoms are seldom apparent at birth, but develop over time
- The impairment is more chronic and delibitating
- Mood dysregulation is random or cyclical, not situational
- Mood is significantly different when not depressed or manic
- Experiences limbic rage, or mood shifts that are rapid, intense, long-lasting, and highly destructive
- Family history of bipolar disorder, or family members who have committed suicide or been institutionalized
- Psychosis, where thinking becomes slippery, delusional, or bizarre
- Destructiveness or violence
- Symptoms respond well to mood stabilizers
Free Winter Holiday Support 2020
60 Days of CPTSD Strategies
One email a day to help you through the holidays!
- Does the thought of the upcoming holiday season cause you anxiety?
- Could you use some help with healthy boundaries, self-care, and making your healing a priority, amidst the chaos?
- Maybe you could just use some extra encouragement during the upcoming holiday season?
- Would a single email per day, containing a video, audio, inspiring quote, or encouraging thought, be something you would find helpful?
If you answered YES to any of these questions, then why not join us for Winter Holiday Support?
Also Check: Does Pristiq Give You Energy
Bipolar Borderline And Ptsd: What’s The Difference
Linnea Butler is the founder of Bay Area Mental HealthDiagnosing mental illness is an imperfect science. trouble sleeping, thoughts of suicide, not being able to maintain relationships, feeling worthless, racing thoughts, inability to focus, low energy, and feeling heightened emotionsSo why does the DSM distinguish between these problems?
How Do We Help Police Officers Address Trauma
Trauma is real, and so is treatment. Several forms of therapy are effective methods for treating trauma. These therapy methods just have to be made standard and accessible. The shame and stigma surrounding getting help needs to be removed. Cops feel like they need to be superheroes. Or they may worry about their job security if they speak up and advocate for their own and others mental health. However, the only way to manage trauma and its effects is to treat it.
The World Health Organization explains that stress management techniques and healthy coping mechanisms, both learned through therapy, are effective tools for immediately responding to stress and its effects. Cognitive Behavioral Therapy and Eye Movement Desensitization and Reprocessing can effectively treat PTSD. The WHO warns against only prescribing medication with no supportive therapy services.2
Medications can cause substance use issues when used as primary treatment regardless of whether or not they are prescribed by health professionals. However many of therapy options for trauma can be integrated with treatment for substance use and addiction.
Donât Miss: Prodromal Symptoms Of Schizophrenia Are Evident
Read Also: What Is The Most Important Predictor Of An Eating Disorder
The Role Of Leadership
PTSD in any form is similar in many ways to a physical injury. Whether a broken arm or PTSD, once the problem is identified and treated, the sufferer can return to a highly functioning life.
In order for officers to identify PTSD symptoms and receive treatment, there must be a change in the culture of law enforcement. Agencies must focus on improving the mental fitness of officers because there is no doubt that PTSD affects a large number of them.
Law enforcement leadership must acknowledge the role PTSD-afflicted officers play in broader public service issues. While data on this subject is lacking information collected by The Marshall Project showed that the few cities that did respond to this data request reported higher rates of excessive force complaints for veterans versus non-veterans .
Ultimately, these are life or death issues , which highlights why it must be a priority for law enforcement leadership. Agencies must provide mental health resources to support both officers and the communities that they serve.
References
Dreazen, Y. . Tour of duty. Foreign Policy, , 52-59.
McCanlies, E. C., Mnatsakanova, A., Andrew, M. E., Burchfiel, C. M., & Violanti, J. M. . Positive psychological factors are associated with lower PTSD symptoms among police officers: Post Hurricane Katrina. Stress & Health: Journal of The International Society For The Investigation Of Stress, 30, 405-415.
Contact Westwind Recovery For Ptsd And Bipolar Disorder Treatment
Westwind Recovery® staff includes seasoned mental health and addiction professionals that believe a human connection and a fun environment are essential components for recovery. They work to help everyone that comes through the door to find a sense of wellness and purpose that starts with a proper diagnosis.
You dont have to live with addiction or a mental health condition like PTSD or bipolar disorder. Contact Westwind Recovery® today at to talk to one of our mental health specialists today.
Read Also: What Is The Phobia For Bees
Other Terms For Complex Ptsd
Complex PTSD is a fairly new term. Professionals have recognised for a while that some types of trauma can have additional effects to PTSD, but have disagreed about whether this is a form of PTSD or an entirely separate condition, and what it should be called.
For example, you may find some doctors or therapists still use one of the following terms:
- enduring personality change after catastrophic experience
- disorders of extreme stress not otherwise specified this term is more common in America than the UK.
“At times I felt nothing was going to end the distress, experiencing more than 10 flashbacks a day… It was a long process of recovery, with lots of bumps along the road, but the right medication and long-term therapy with someone I came to trust, has changed my life.”