Symptom Categories In Schizophrenia
Generally, symptoms are classified as
- Positive: a distortion of normal functions
- Negative: a decrease or loss of normal functions and affectivity
- Disorganised: disturbances in thinking and bizarre behaviour
- Cognitive: deficits in information processing and problem solving
Patients may experience symptoms in one or more categories.
Positive symptoms can be further classified as
- Delusions
Delusions are erroneous beliefs that are maintained despite clear contradictory evidence.
There are several types of delusions:
- Persecutory delusions: patients believe they are being harassed, followed, cheated or spied on.
- Reference delusions: Patients are convinced that passages from books, newspapers, song lyrics or other environmental stimuli are directed at them.
- Delusions of theft or thought graft: patients believe that others can read their minds, that their thoughts are being transmitted to others, or that thoughts and impulses are being imposed on them by external forces.
Delusions in schizophrenia tend to be bizarre, i.e., implausible and not derived from common life experiences .
Hallucinations are sensory perceptions that are not perceived by anyone else.
They may be auditory, visual, olfactory, gustatory or tactile, but auditory hallucinations are by far the most common.
Patients may hear voices commenting on their behaviour, conversing with each other or making critical and hurtful comments.
Delusions and hallucinations can be extremely irritating for patients.
Stress And Children Trauma
One study found that 59 percent of males and 69 percent of females hospitalized for schizophrenia suffered childhood trauma including physical and emotional abuse. Other stress can include head injury, family breakdown, or a death in the family. In addition, children whose mothers experienced severe stress or mental disorders while pregnant had a higher risk for developing schizophrenia.
Diagnosing Psychosis In Children And Teenagers
Many of the symptoms of psychosis in adults arent symptoms of psychosis in young people. For example, small children often have imaginary friends with whom they talk. This just represents imaginative play, which is completely normal for children.
But if youre worried about psychosis in a child or adolescent, its best to describe their behavior to a doctor.
Treating psychosis may involve a combination of medications and therapy. Most people will experience an improvement in their symptoms with treatment.
Don’t Miss: How To Get Motivated To Workout When Depressed
Prenatal Risk Factors In Schizophrenia
Ezra S. Susser, MDPsychiatric Times
Significant research developments in the etiopathogenesis of schizophrenia have occurred during the past several years. One such advance is the “neurodevelopmental” hypothesis that events during early brain development, especially the prenatal and perinatal periods, may play an important causal role in at least some, and perhaps many, cases of schizophrenia.
Can Schizophrenia Be Treated
Yes. The main types of treatment are counseling and medicines to lessen or stop psychotic symptoms. Medicines will control psychotic symptoms in most people. In milder cases of schizophrenia, medications may not be needed. Medicines can:
- Lessen or stop hallucinations
- Help the person tell the difference between hallucinations and the real world
- Lessen or stop false beliefs
- Lessen feelings of confusion
- Help the person think more clearly
Lessening of these symptoms can help the person resume his or her normal lifestyle and activities. Medicines for schizophrenia need to be taken regularly, even after symptoms are gone. Some people with schizophrenia will stop taking their medicine because they believe the medicine is no longer needed, or they dislike the medication’s side effects. Psychotic symptoms often return when medication is stopped. Do not stop taking medicine without the advice of your healthcare provider.
Discuss any concerns you have about side effects with your healthcare provider.
Recommended Reading: Hippopotomonstrosesquipedaliophobes.
Infections And Immune System
A number of viral exposures during prenatal development, have been associated with an increased risk of schizophrenia. Schizophrenia is somewhat more common in those born in winter to early spring, when such infections are more common.
Influenza has long been studied as a possible factor. A 1988 study found that individuals who were exposed to the Asian flu in the second trimester were at increased risk of later developing schizophrenia. This result was corroborated by a later British study of the same pandemic, but not by a 1994 study of the pandemic in Croatia. A Japanese study also found no support for a link between schizophrenia and birth after an influenza epidemic.
Polio, measles, varicella-zoster, rubella, herpes simplex, maternal genital infections, Borna disease virus, and Toxoplasma gondii have been correlated with the later development of schizophrenia. Psychiatrists E. Fuller Torrey and R.H. Yolken have hypothesized that the latter, a common parasite in humans, contributes to some cases of schizophrenia.
In a meta-analysis of several studies, they found moderately higher levels of Toxoplasma antibodies in those with schizophrenia and possibly higher rates of prenatal or early postnatal exposure to Toxoplasma gondii, but not acute infection. However, in another study of postmortem brain tissue, the authors have reported equivocal or negative results, including no evidence of herpes virus or T. gondii involvement in schizophrenia.
Other factors
Risk Factors For Suicide In Patients With Schizophrenia
Risk Factors for Suicide in Patients With Schizophrenia
It has long been known that persons with schizophrenia are at high risk for attempted and completed suicide. With estimates of about 5% to 15% for completed suicide1,2 and 20% to 40% for attempted suicide,3-6 the recent increase in attention to this concern is promising. Most studies have involved reviews of patient charts and reviews of psychiatric and death registries, which limits our understanding of risk factors, warning signs, and potential interventions. More recently, the assessment of suicidal behavior in patients with schizophrenia in clinical trials has added a new dimension to the research.7 Prospective longitudinal studies that directly assess baseline history of suicidal behavior and related factors will be the most informative.
Risk of completed suicide and of attempted suicide may be different. In addition, some risk factors cut across psychopathologies and some are unique to individuals with schizophrenia and schizoaffective disorder. The following is a review of the risk factors for sui-cidal behavior in patients with schizophrenia where possible, the differentiations between those who attempt suicide and those who complete suicide will be made .
Previous suicidal behavior As with most disorders, the best predictor of future behavior is past behavior. In schizophrenia, almost half of suicide completers have made a previous attempt12 and attempters typically make more than one attempt.6
Read Also: The Phobia For Long Words
People With Schizophrenia Are Nearly Three Times More Likely To Die Of Coronavirus Infection Than Those Without The Psychiatric Disorder
People with schizophrenia, a mental disorder that affects mood and perception of reality, are almost three times more likely to die from coronavirus disease than those without the psychiatric illness, a new study shows. Their higher risk, the investigators say, cannot be explained by other factors that often accompany serious mental health disorders, such as higher rates of heart disease, diabetes, and smoking.
Led by researchers at NYU Grossman School of Medicine, the investigation showed that schizophrenia is by far the biggest risk factor after age . Male sex, heart disease, and race ranked next after schizophrenia in order.
Our findings illustrate that people with schizophrenia are extremely vulnerable to the effects of COVID-19, says study lead author Katlyn Nemani, MD. With this newfound understanding, healthcare providers can better prioritize vaccine distribution, testing, and medical care for this group, adds Dr. Nemani, a research assistant professor in the Department of Psychiatry at NYU Langone Health.
The study also showed that people with other mental health problems such as mood or anxiety disorders were not at increased risk of death from coronavirus infection.
They note that this large sample of patients who all were infected with the same virus provided a unique opportunity to study the underlying effects of schizophrenia on the body.
Study funding was provided by NYU Langone.
What Role Do Epigenetic Factors Play In Schizophrenia And Could This Affect Brain Development
As previously mentioned most genetic variance in schizophrenia is in non-coding, potentially regulatory areas of the genome. In general, during development the more well-studied epigenetic processes such as DNA methylation and histone acetylation control the availability of the local chromatin environment for transcription and along with small non-coding RNA species help cells to maintain a differentiated state,. Here, I will discuss the epigenetic factors implicated in schizophrenia which may also have implications for developing brains.
In general, the genome becomes progressively more methylated with age. This has been recently confirmed for genes related to brain development, i.e. neuron differentiation and axonogenesis in the human prefrontal cortex . However more importantly when these authors examined CpG sites within schizophrenia GWAS-implicated variants, this CpGs were more highly methylated and this finding was driven by sites that were more heavily methylated in foetal compared with adult life. Importantly, reanalysis of such methylation patterns in adult PFC from patients with schizophrenia showed no such association. This work was largely replicated by a separate group that found the GWAS-significant loci were more than four times likely to be methylated in the foetal brain compared to regions unrelated to schizophrenia.
Recommended Reading: Phobia Meaning
Hypothesis: Social Defeat Is A Risk Factor For Schizophrenia
Published online by Cambridge University Press: 02 January 2018
- Department of Psychiatry, Rudolf Magnus Institute of Neuroscience, University Medical Centre Utrecht, Utrecht, the Netherlands
- Elizabeth Cantor-Graae
- Affiliation:Department of Health Science, Section for Social Medicine and Global Health, Lund University, University Hospital UMAS, Malmö, Sweden
- *
- Dr. J. P. Selten, Department of Psychiatry, UniversityHospital, P.O. Box 85500, 3508 GA Utrecht, The Netherlands. Email:
What Are The Symptoms Of Schizophrenia
Schizophrenia has a large variety of symptoms and can seem very different in one person from another. If its not treated, schizophrenia may lead to long-term psychosis.
The main symptoms of schizophrenia are:
- hallucinations
- delusions
- confused thinking: thoughts are jumbled and the person cant make sense of what other people are saying.
Someone with schizophrenia will have symptoms for more than 6 months. They may have unusual ideas or beliefs about themselves or the world around them, which may be frightening.
You May Like: Faratraphobia
Summary And Future Directions
Several environmental exposures have been investigated in terms of SZ and BD risk, and there is moderate evidence that ACEs and certain types of infections are risk factors for both. For winter/spring birth, OCs, migration, urbanicity, and cannabis use, however, more robust associations have only been identified for SZ. Undoubtedly, the research for BD lags behind the larger body of work for SZ, and it remains unclear whether the reported differences in environmental risk between BD and SZ are due to sample size and methodological differences, or true etiological distinctions. For both disorders, evidence implicating other exposures such as air pollution and nicotine/smoking is still growing, while still other exposures may yet be discovered. Only a small fraction of environmental variables that individuals are exposed to have been investigated, and, in time, more environmental risk factors for SZ and BD will likely come to light.
Power has been another key limitation of most prior G×E research. Power calculations using sample sizes from previous G × E studies suggest that some of the reported results may represent false positives . As larger samples become available, well-powered interaction studies will become feasible.
Some Models Produce Early Alterations In Gaba/glutamatergic Systems
Many of these developmental RFs also affect GABA and glutamate function in adult offspring. However, there is minimal data on how these RFs affect the early development of these neurotransmitter systems. Perhaps the best evidence comes from studies of prenatal hypoxia. Prenatal hypoxia alters embryonic cortical GABA cell number and positioning up to P2 in the cortex but this reverses from P4. Prenatal hypoxia at GD17 in mice also induces an immediate reduction in foetal cerebral cortex levels of the GABA synthesising enzyme, glutamate decarboxylase. Prenatal hypoxia also upregulates the NR1 subunit of the NMDA receptor for up to 3 days post exposure in white matter microglia but this is reversed from 7 days post exposure.
There is no evidence of effects of MIA on glutamate and GABA systems in the developing brain. Effects on adult brain however are clearly dependent on the timing of exposure. While MIA has no long lasting effect on glutamate or GABA levels, exposure at later gestational ages such as GD17 leads to alterations in GABA and NMDA NR1 subunit expression in juveniles and adult offspring,,. Earlier gestational exposures, however, have little to no effect on this neurotransmitter systems.
Read Also: Childhood Trauma And Bipolar Disorder
Disturbances Of Early Development
Prospectively collected measures of premorbid function have consistently revealed neuromotor abnormalities and developmental delays. In the British 1946 Birth Cohort pre-schizophrenic children were found to have delayed motor and speech development by the age of 2 years. In the Northern Finland 1966 Birth Cohort the ages that children learned to stand, walk and become potty-trained were related to subsequent risk for schizophrenia and other psychoses earlier milestones reduced the risk, whereas later milestones increased it. Cannon et al.showed, in a birth cohort from New Zealand, that children who went on to develop schizophreniform disorder had persistently poor motor function over repeated measurements in childhood. In an innovative study using home movies filmed during childhood, pre-schizophrenic individuals could be differentiated from their healthy siblings by viewers who were blind to the psychiatric outcomes.
Which Risk Factors Are Associated With Schizophrenia
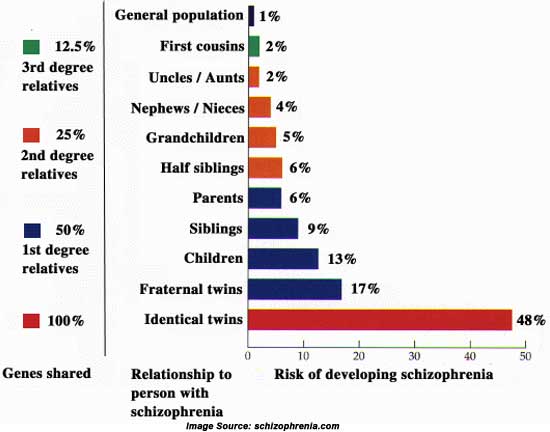
Many disorders are the result of interaction between genetic and environmental influences. One example is cardiovascular disease people with a family history of cardiovascular disease are more susceptible to heart problems, and environmental influences such as poor diet can increase this risk. Schizophrenia is also a complex disorder that can arise from both genetic and environmental influences, although genetic factors contribute a much greater risk than environmental factors with a heritability estimate of 80%.
We have not included detailed information on genetic risk factors in the Library due to the availability of these details on a website specifically about genetics in schizophrenia .
Several environmental risk factors have been identified as increasing the risk for schizophrenia, these include:
- Recreational cannabis use, particularly in childhood or adolescence.
- Exposure to obstetric complications in utero or at birth, including maternal diabetes, emergency caesarean section, congenital malformations, or low birth weight < 2000g.
- Exposure to severe childhood adversities, and poor family relationships.
- Being an immigrant, either first or second generation, particularly from a developing country coming to a developed country and living in an area with low ethnic minority density.
- Exposure to childhood central nervous system viral infections.
- Having an older father at birth.
Don’t Miss: What Is The Phobia Of Throwing Up Called
Social Class And Isolation
Some reports link social inequality at birth with schizophrenia. Socioeconomic status has been reported to be associated with an increased risk of psychosis . However, while some findings are positive, there are a number of conflicting studies showing no association between psychosis and low social class at birth or even a link with high social class .
What Is Paranoid Schizophrenia
Paranoid schizophrenia is one type of schizophrenia. In this type, the person’s false beliefs are mainly about being persecuted or being punished by someone. The person may hear the voice of someone he or she believes is punishing them. The person may believe that he or she has been specially chosen to complete a secret mission. These are just a few examples of any number of false beliefs a person with this disorder may have.
Other types of schizophrenia include “catatonic” schizophrenia and “disorganized” schizophrenia. Different types of schizophrenia may have some of the same symptoms.
You May Like: Feretrophobia
Premorbid Cognitive And Scholastic Performance
Schizophrenia patients, when considered as a group, have intellectual impairments, some of which predate the onset of psychotic symptoms. Individuals who later develop schizophrenia have been found to perform below average on standardized measures of intelligence in childhood, adolescence and young adulthood, and to show lower premorbid IQ than the general population The lower the IQ, the higher is the risk for later development of schizophrenia.
Poor school performance can be seen as a premorbid sign. Repeating a grade, difficulties in completing the final level of schooling, and social and behavioural difficulties have also been found to be risk factors for developing schizophrenia. In the Northern Finland 1966 Birth Cohort, 14-year-olds who were below their expected normal grade were three times more likely to develop schizophrenia than those in their normal grade, but low school marks did not predict schizophrenia. Developmental continuity, indicated by early developmental deviation in the first year of life associated with lower school performance at age 16 years, has been found to be stronger among children who develop psychoses later in life than among normal controls and those admitted to hospital for non-psychotic psychiatric disorder.
Other Family Environmental Factors
In the British 1946 Birth Cohort, schizophrenia in offspring has been linked with problems in mothers general understanding and management of their children . Goldstein concluded that communication deviance in the family increased the risk for schizophrenia. Having a positive relationship with both the mother and father might be protective against schizophrenia among high-risk children. These findings may be explained by geneenvironment interaction.
In Finnish studies some possible stress factors have not generally been linked to schizophrenia. Very early temporal separation from parents and transfer to adequate nursing homes immediately after birth because of tuberculosis in the family did not predict schizophrenia, and neither did living in a single-parent family in childhood, low socio-economic status, or the size of the family of origin and multiparity. The connection between childhood socio-economic status and schizophrenia is not yet entirely resolved. Low or high socio-economic status in the family of origin has been found to be at least a modest risk factor for schizophrenia in some studies, while other studies report no increased risk.
Don’t Miss: Pristiq What Is It Used For