Signs And Symptoms Of Paranoid Schizophrenia
Signs and symptoms of paranoid schizophrenia include:
- Auditory hallucinations hearing things that are not there
- Delusions false beliefs
- Anxiety this may appear in periods of high levels of anxiety
- Anger may start mild but range in severity. Anger can raise blood pressure, heart rate, and adrenaline.
- Detachment either physically or emotionally detached from others
- Aggression and violence aggression may contribute to violent outbursts
- Quarrels
- Condescension patient may believe they know stuff that others do not, so they come off as patronizing
- Suicidal thoughts and behavior patient may say phrases such as I wish I was never born, or go out of their way to find weapons or pills to kill themselves with. Early warning signs of suicide include social withdrawal, mood swings, obsession with dying or violence, feeling trapped or desperate, illicit drug usage, changes in eating or sleeping patterns, getting ones affairs in order, and saying goodbye to people in a specific way.
You May Like: Does Celine Dion Have An Eating Disorder
Main Outcome Measure And Definition
Diagnoses of dementia were obtained from the DPCR and the DNPR . Diagnoses of the main outcome Alzheimer’s dementia were obtained . The date of dementia onset was defined as the first day of hospital contact with a diagnosis of dementia in either the DPCR or the DNPR . All analyses were also performed for vascular dementia and unspecified dementia .
Studies Showing A Significant Decline In Cognition Over Time
In a re-evaluation of the IOWA 500 study of a cohort of people with hebephrenic or catatonic schizophrenia followed up for 40 years, Reference Winokur, Pfohl, Tsuang, Miller and CohenWinokur et al found that the subgroup of older participants was significantly more likely to have worsened orientation and memory.
Don’t Miss: What Is The Fear Of Long Words Called
Data Abstraction And Quality Assessment
The two authors independently extracted the data. If there was disagreement, a colleague was consulted to resolve the disagreement. The following data were extracted from each study: the first authors family name, year of publication, study design, country, location, number of participants, number of dementia cases, sex, mean age, follow-up time, assessment of schizophrenia and dementia, adjusted covariates, and study quality. The NOS criteria were used to evaluate the quality of the included original articles. The quality of studies was evaluated in the following three major components: selection of the study group , quality of the adjustment for confounding , and assessment of outcome or exposure in the cohorts . Studies were graded on a high to low point scheme, with a good quality score if they met 78 points, fair if they met 46 points, and poor if they met 4 points.
Patterns Of Regional White Matter Deficits In Ad Mci And Sz
Five samples were analyzed to test the above hypothesesthe ADNI samples for AD and MCI and 3 SZ samplesa discovery sample from Baltimore, MD a replication sample from Beijing, China and a replication sample from the worldwide meta-sample from ENIGMA, which is the largest white matter imaging sample in SZ. Each sample had its own healthy controls. Details on sample size, demographic , and imaging information are in the Methods section and supplementary information. White matter microstructures were measured by FA of DTI. The ranks of regional FA effect sizes between patients and controls for each cohort are shown in and supplementary table S4. In AD, the largest effect sizes were in the fornix followed by the splenium of the corpus callosum . In MCI, the largest effect sizes were in the SCC and FX . In the 3 SZ cohorts, patients showed the largest effect sizes in the anterior corona radiata , anterior limb of the internal capsule , FX, and body of the corpus callosum . The regional patient-control effect sizes in the discovery and replication cohorts were significantly correlated with those reported by ENIGMA .
Read Also: Fear Of Spoons Phobia Name
Brain Imaging And Diagnosis
Technological advances have led to a greater use of structural and functional brain imaging to assist with the diagnosis of dementia in people with evidence of cognitive decline. Additional information obtained from these investigations helps clinicians to make an accurate diagnosis and formulate a treatment plan. In clinical practice, structural magnetic resonance imaging and computed tomography scanning are widely used, and radiologists interpret results on the basis of visual readings.
Structural imaging is often carried out to identify potentially treatable causes of dementia, such as normal pressure hydrocephalus or space-occupying lesions, or to clarify the diagnosis by detecting cerebral infarctions or patterns of atrophy. In cognitively impaired patients without a definite clinical diagnosis, MRI may be helpful in reaching a diagnosis. Without MRI investigation the clinical diagnosis of vascular dementia may be unreliable. Image analysis programs that quantify regional volumes in MRI have shown that measures of medial temporal or hippocampal atrophy can distinguish people with Alzheimers disease from controls. Several studies have shown ventricular enlargement, cerebral infarction or white matter ischaemic change using CT or MRI scans. However, these findings are non-specific in both Alzheimers disease and vascular dementia.
For a summary of this section, see Box 5.
BOX 5 Brain imaging
Little is known about functional imaging in this area.
Prognosis Of Dementia In Schizophrenia
Dementia shortens the lifespan. At any given age, people who have dementia are two to four times more likely to die than those who do not have the disease . The median survival time of people with dementia has been investigated in cohort studies and case series in various settings, and it ranges from 3 to 9 years . However, longitudinal comparisons of the course of cognitive and functional decline have been very few in the subpopulation with dementia in schizophrenia. Reference MayerMayer found that many of Kraepelins patients with paraphrenic psychoses showed unequivocal signs of dementia later in the course of illness. Reference HoldenHolden observed that people with late paraphrenia had significantly worse outcomes when they developed dementia.
As mentioned earlier, Reference Goldberg, Hyde and KleinmanGoldberg et al stated that schizophrenia can be regarded as a static encephalopathy. Some studies suggest that the progressive cognitive decline experienced by people with poor-outcome schizophrenia is not a linear process across the lifespan, and the rate of decline may accelerate after the age of 65 .
Again, more studies are needed, on both the survival rates and prognosis of people with schizophrenia once they develop dementia .
BOX 8 Prognosis
Dementia shortens life more than schizophrenia
The median survival for people with dementia is 39 years, and it decreases significantly with age
You May Like: Which Of The Following Is The Most Important Predictor Of An Eating Disorder
Emergence Of Psychosis In Later Life
An important and ongoing issue is the relationship between the emergence of psychotic symptoms in later life and the risk of incident cognitive decline and dementia. As reflected in the Jeste and Finkel criteria for psychosis in AD, psychotic symptoms were included only when they emerged after a dementia diagnosis. However, psychotic symptoms have been observed in people with MCI. Specifically, hallucinations are present in 1.32.6% and delusions in 3.110.5% of patients with MCI. Most,,, but not all, longitudinal studies have found an increased risk of dementia associated with psychosis. For the negative studies, low baseline psychosis frequency in the study sample and short median duration of follow-up might have been confounding factors. Although more research is required, the evidence to date suggests that psychosis in MCI is part of the neurodegenerative disease process, supporting the inclusion of MCI or mild neurocognitive disorders in the new IPA criteria.
Neurobiological data are also emerging to link late-life psychosis to neurodegeneration. For example, a post-mortem study has shown an association between argyrophilic grain disease a four-repeat tauopathy and psychosis in individuals aged 65 years. In this age group, people with psychosis had sixfold increased odds of having this neurodegenerative condition compared with non-psychiatric controls.
The Western Mind And The Concept Of Dementia
At certain stages of civilization, each culture develops an elaborate concept of thenature of the mind and how it relates to the worlds of spirit andfleshi.e., the organs, or bodily systems, which uphold theworkings of the mind.1 The Westernconcept of the mind has its roots in Antiquity, but it was only in the XVIII centurythat it crystallized into a coherent theory.2 Accordingly, the mind is conceived as a tripartite entitycomposed of conation, cognition, and affectivity. Together, these compartmentsentail the fundamental structure of the human psyche, consisting, respectively, ofthe inclination to act upon the world , the means to attend to, store andoperate upon relevant information in the environment , and the endowment of ideational and exteroceptiveevents with personal relevance, which is typically accompanied by changes inviscero-autonomic activity . Thisconcept has explicitly-or, more often, implicitly-framed all aspects of present-dayneurological and psychiatric thought.
You May Like: Can Dehydration Cause Anxiety Attacks
The Risk Of Dementia In Late
Late-onset schizophrenia is usually defined as onset after 40 years of age, and very-late-onset as after 60 years of age. Studies of schizophrenia of late and very late onset are few and inconsistent in their results.
Reference Palmer, Bondi and TwamleyPalmer et al compared changes in cognition over 1 and 2 years for out-patients with late-onset schizophrenia-spectrum disorders, earlier-onset schizophrenia-spectrum disorders, Alzheimers disease with psychosis, or Alzheimers disease with baseline MMSE scores > 25, and healthy comparison participants. Cognitive changes among participants in the two schizophrenia-spectrum disorder groups were similar to those in the healthy controls, whereas both Alzheimers disease groups showed greater declines in cognition. The authors concluded that late-onset schizophrenia is a neurodegenerative disorder and, in agreement with earlier studies, a static encephalopathy.
This Danish study suggests that, although people with late-onset and very-late-onset schizophrenia have an increased risk of developing dementia, it does not seem to be due to an increased risk of developing Alzheimers disease, thus pointing to the possibility that they are developing a different type of dementia.
Box 1 summarises the evidence from international studies.
BOX 1 Cognitive impairment in schizophrenia
Cognitive impairment is a feature of schizophrenia
Over 25% of older people with schizophrenia have moderate to severe cognitive impairment
Studies Showing A Lesser Decline In Cognition
An early study of older in-patients with schizophrenia demonstrated that cognitive changes were very slow over time, despite low MMSE scores at initial assessment. The authors concluded that cognitive functioning in older people with schizophrenia is different from that seen in Alzheimers disease.
Reference Heaton, Paulsen and McAdamsHeaton et al compared three groups of people with schizophrenia with ambulatory patients with Alzheimers disease and normal controls. They concluded that cognitive impairment in schizophrenia is unrelated to current age, age at onset or duration of illness. They also suggested that there is an encephalopathy associated with schizophrenia that is non-progressive and that has a different pattern of deficits from that seen in Alzheimers disease.
You May Like: Which Organization Sets The Standards For Diagnosing Eating Disorders
Positive Symptoms Of Schizophrenia
In this case, the word positive doesnât mean good. It refers to added thoughts or actions that arenât based in reality. Theyâre sometimes called psychotic symptoms and can include:
- Delusions: These are false, mixed, and sometimes strange beliefs that arenât based in reality and that the person refuses to give up, even when shown the facts. For example, a person with delusions may believe that people can hear their thoughts, that they are God or the devil, or that people are putting thoughts into their head or plotting against them.
- Hallucinations: These involve sensations that arenât real. Hearing voices is the most common hallucination in people with schizophrenia. The voices may comment on the personâs behavior, insult them, or give commands. Less common types include seeing things that arenât there, smelling strange odors, having a funny taste in your mouth, and feeling sensations on your skin even though nothing is touching your body.
- Catatonia: In this condition, the person may stop speaking, and their body may be fixed in a single position for a very long time.
Risk For Dementia Is Increased For Individuals With Schizophrenia
Schizophrenia is a chronic disorder characterized by symptoms that include hallucinations, delusions, abnormalities in the verbal expression of thought, diminished social interactions, diminished motivation, and difficulties with cognitive tasks involving attention, memory, and planning. The long term course of this disorder varies. Some individuals, with the help of appropriate medication and social support, can live independently, be employed, and enjoy friends and hobbies. For others, however, the symptoms are difficult to manage and interfere with most aspects of their lives, often leading to disability and early death. It is also not uncommon for persons with schizophrenia to use street drugs and alcohol, and chronic abuse of alcohol or illicit drugs negatively impacts their long-term outcome.
Although cognitive symptoms involving attention and memory are common in persons with schizophrenia, such symptoms tend to be stable and non-progressive through middle age. Whether schizophrenia is associated with an increased risk for a progressive dementia later in life has been the focus of several research studies, but the results so far have been inconclusive. Prospective studies addressing this issue are difficult to perform given the need for a large study population and the long period of time between an initial diagnosis of schizophrenia and the onset of dementia.
Read Also: Mania And Phobia List
Does Schizophrenia Get Worse As You Age
For some people, schizophrenia symptoms and episodes may grow worse with time or age, particularly if they avoid treatment or professional help. However, when schizophrenia manifests at a younger age, symptoms and behavior are generally more extreme than with later-onset schizophrenia. That means if schizophrenia symptoms develop later in life, theyre generally less severe than when they develop at a younger age.
The most important thing to remember is that schizophrenia doesnt necessarily get worse with age. Preliminary research has found that individuals living with schizophrenia dont experience cognitive decline any faster than the general population. Psychosocial function may even improve with age, and most individuals experience improved quality of life as they grow older.
For people committed to recovery and following a medication regimen, a long-term balanced lifestyle is possible with preventative treatment, even as they grow older.
Are you or someone you care about struggling with symptoms of schizophrenia? Find out if PCH is the right place to find the help and hope youre looking for. Is PCH Right for You?
Mental Illness Tied To Increased Dementia Risk
Batya Swift Yasgur, MA, LSW
Mental disorders in early life are associated with a significantly increased risk of dementia in later years.
Results of a large, longitudinal, population-based study show that individuals hospitalized for a mental health disorder had a fourfold increased relative risk for developing dementia compared to those who were not hospitalized with a mental illness.
In addition, those with dementia plus a mental disorder developed dementia almost 6 years earlier than those without a mental illness.
The findings were consistent among men and women, in patients with early- and late-onset dementia, in those with Alzheimer’s and non-Alzheimer’s dementia, and across all mental health disorders and remained so after accounting for preexisting physical illness and socioeconomic factors.
“Dementia is not typically treated until later in life, but our study suggests that we need to be thinking about dementia prevention much earlier in the life course,” study investigator Leah Richmond-Rakerd, PhD, assistant professor, Department of Psychology, University of Michigan, told Medscape Medical News.
“Supporting young people’s mental health could be a window of opportunity to help reduce the burden of dementia in older adults,” she said.
The findings were February 16.
Also Check: Does Pristiq Work For Anxiety
The Status Of Dementia Prcox In The Era Of Schizophrenia
Dementia is no longer an obligatory symptom of schizophrenia. However, this wasnot always so. Indeed, the first successful taxonomic scheme envisaged dementiaas the core defining symptom of this intriguing disease. The roots of theconcept of schizophreniaa form of dementia that set in during adolescence orearly adulthoodwere established by the end of the XIX century. First andforemost was the keen observation that the early dissimilar conditions such ascatatonia16 andhebephrenia17 sharedan unfavorable long-term prognosis. This formulation obviously depended on athorough documentation of the natural course of apparently unrelated clinicalstates when viewed cross-sectionally, but which converged into a terminaldementia if enough time for observation was allowed, usually several years. Thisprognostic criterion led Kraepelin, from 1893 to 1904, to unify them under therubric of dementia præcox.18
Frontotemporal Dementia Manifested As Schizophrenia With Decreased Heterochromatin On Chromosome 1
Philippos Gourzis
1Department of Psychiatry, School of Medicine and University Hospital of Patras, University of Patras, 26504 Rio, Patras, Greece
2Department of Neurology, School of Medicine and University Hospital of Patras, University of Patras, 26504 Rio, Patras, Greece
3Department of Chemistry, Laboratory of Biochemistry, University of Patras, 26504 Rio, Patras, Greece
4Department of Genetics, Alexandra Hospital, 10671 Athens, Greece
Academic Editor:
Abstract
1. Introduction
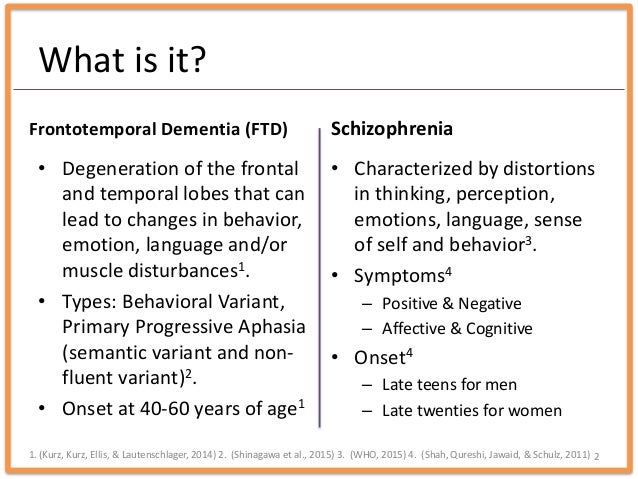
Frontotemporal dementia is a mainly presenile degenerative disorder marked by progressive behavioural changes and cognitive impairment, characterized by progressive atrophy of both frontal and anterior temporal lobes . The disease has now been proved as the second most common type of presenile dementia, with a correlation ratio of about one case of FTD to four of Alzheimers disease . An autosomal dominant pattern of inheritance is found in 1027% of all FTD patients , with several genetic defects identified in some, but not all, hereditary cases of FTD .
Differentiation between FTD, primary psychiatric disorders, AD, and other dementias is crucial for case management and determining prognosis. Identification of factors relating to etiology, age of onset, and clinical presentation of FTD could help expand our understanding of the pathogenesis of the disorder, and probably enhance accurate clinical diagnosis .
2. Case Presentation
3. Discussion
Abbreviation List
Consent
References
Copyright
Don’t Miss: Sex Differences In Depression